One of the best pieces of news for me has been young Daimler Hamlin’s announcement that he is fit to resume playing American football. The young man had collapsed on the field not too long ago after receiving a chest blow from an opponent. There are multiple videos confirming the blow to the chest and Hamlin collapsing soon after. Luckily for him, there were paramedics around who defibrillated him. There is news that he needed more than a couple of DC shocks. He was transferred to a hospital for the necessary observation and management. We have no access to the investigations done, and rightly so.
Many cardiologists suggested that this was a clear-cut case of vaccine-induced myocarditis-induced sudden death syndrome because of the vaccine mandate in his football league. There have been multiple reports of young people, especially men, collapsing on the playing field, with some sadly dying.
In the case of Hamlin, the presentation is quite different; there is a definite blow to the chest, following which Hamlin collapses after a few seconds. The sequence of events confirms Commotio Cordis. The unfortunate blow was timed to perfection, some milliseconds before the peak of the T wave, and with sufficient force to trigger a polymorphic ventricular tachycardia that soon degenerated into ventricular fibrillation.
On the sporting field, commotion cordis is seen more commonly in men than in women; the explanation given is that men may have a lower threshold or reserve during the depolarization phase. However, outside of the sporting field, more women suffer than men. The situations leading to Commotio Covid could be a motor vehicle accident, a brawl, or some accident in which the chest is struck by some object.
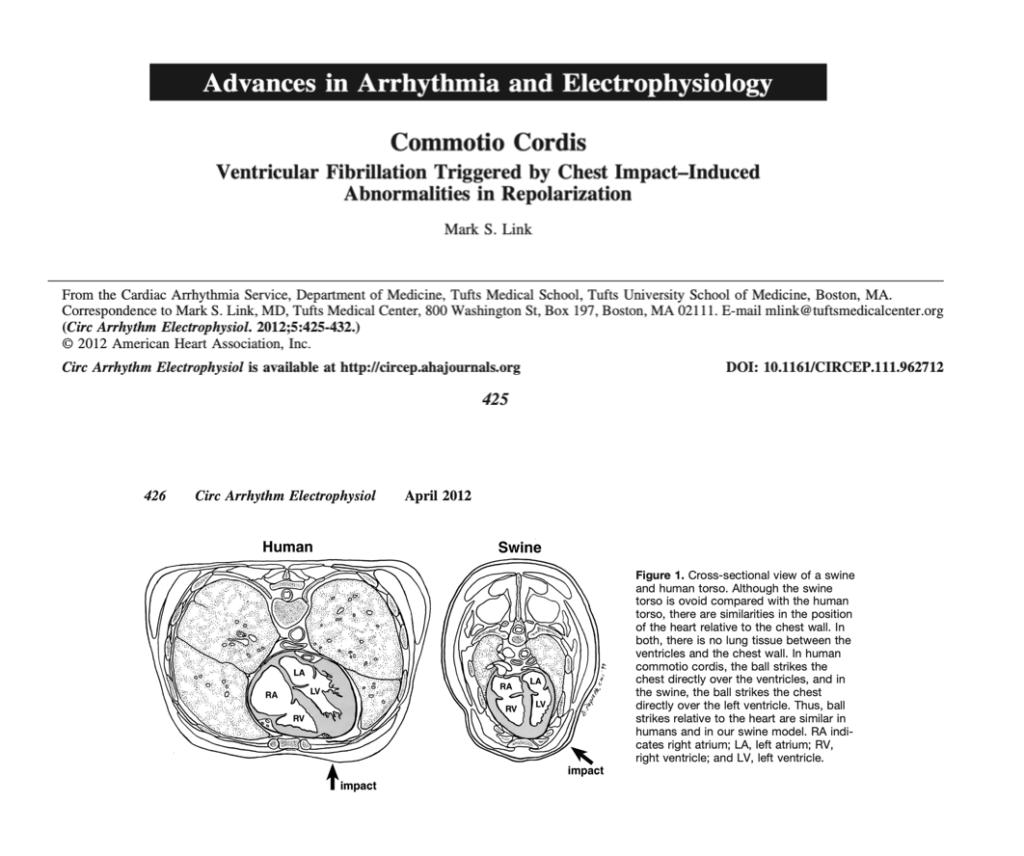
Experiments in animals have revealed that in a 20-kg swine, a pressure impact of 300 mmHg to 500 mmHg at a speed of 30 to 50 mph would be enough to trigger an unstable heartbeat or a ventricular tachyarrhythmia. The timing of the impact is crucial; it should be during the vulnerable period just before the T wave of the ECG peaks. This could be 30 to 40 milliseconds earlier.
There is little tissue between the human heart and the breastbone or the ribs. The bones in the young are still in development, hence Commotio Cordis is most often reported in teenagers aged 16–17 years. An underdeveloped sternum makes the heart more susceptible to a lethal physical impact.
Any sport entailing physical contact or the hurling of a hard ball can lead to an incident. Baseball is a good example, where a firm and hard ball is thrown towards the batter. There can always be a chance of the ball being missed by the baseball bat and striking the batter’s chest. The game of cricket is different. The cricket ball has to hit the pitch first before bouncing off towards the stumps. The chances of the cricket ball hitting the chest of the batter are therefore considerably diminished. The cricket ball after pitching usually stays knee high, but a bowler could deliberately bowl a bouncer aiming at the head or chest of the batter.
Some years ago, The Lancet published a case report of a 25-year-old engineer who was struck by a cricket ball on his chest; he collapsed about 30 seconds later. Luckily, CPR was initiated, and defibrillation was performed as late as 9 minutes after the collapse. The batter regained consciousness, and there were no changes in his ECG, 2-D echocardiogram, or even MRI. The engineer resumed playing cricket after three months.
I had written an article for the Wire on the need for the Indian cricket team to wear a chest protector. The article was written during the last Border Gavaskar test series between India and Australia, which took place in Australia. India won the series despite the Australian fast bowlers deliberately aiming for the bodies of the Indian batters. There is no proof that a chest protector will make one foolproof against Commotio cordis, but it just might mitigate the impact.
I would bet that Hamlin suffered from commotio cordis despite being fully vaccinated. For all practical purposes, the vaccine must have been of the mRNA type. For all you know, he could even have underlying myocarditis or heart inflammation because of the vaccine. There is yet another possibility: that he suffered a viral myocarditis some years ago and carries a scar in his heart due to that inflammation. There are case reports of people suffering from commotio cordis over an underlying old myocarditis scar. The scar tissue could serve as a substrate or sensitise the trigger for a dangerous ventricular arrhythmia. This could also occur after an mRNA vaccine-induced myocarditis.
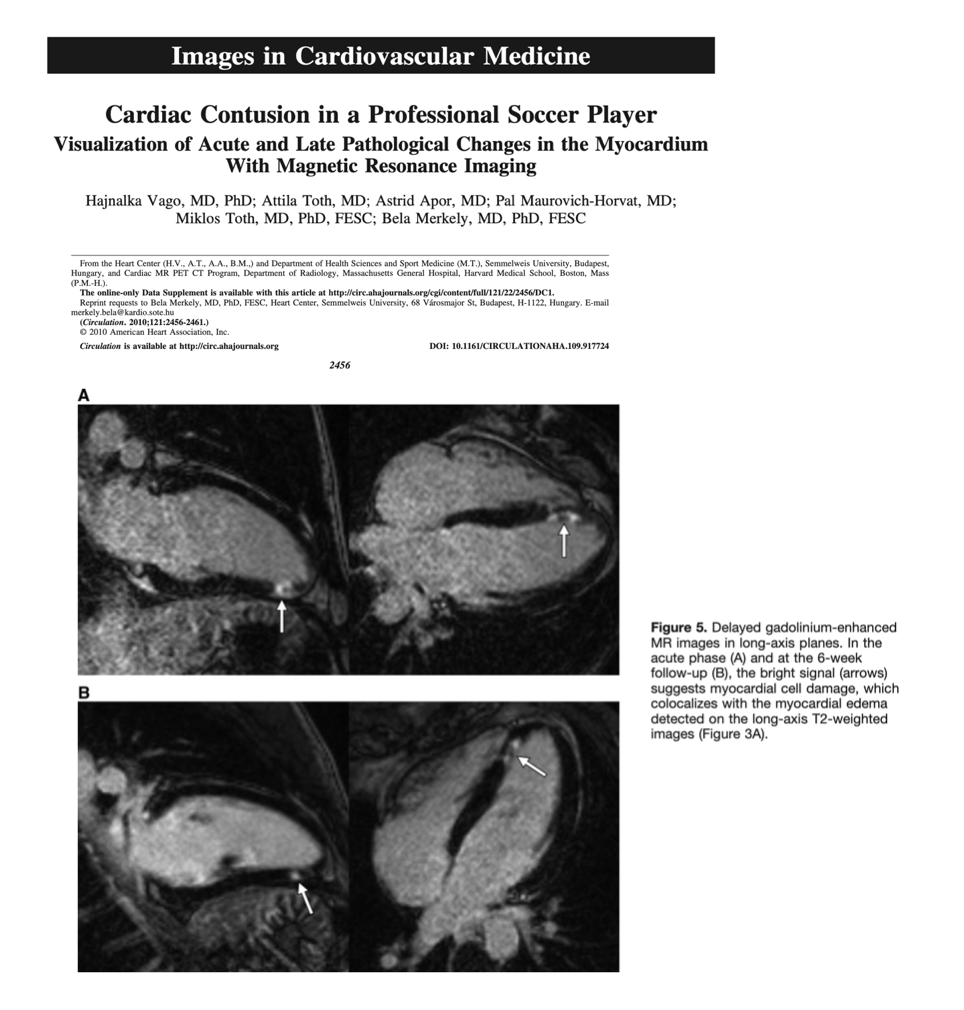
So what do we conclude? The answer is difficult from the outside. The working diagnosis will be commotio cordis because the collapse occurred very soon after being struck in the chest. A cardiac MRI would be of great help in confirming what actually took place. The cardiac MRI may not be definitive if done after 3 months, but if it was done when Hamlin was hospitalised, it could display edoema and haemorrhage in the left ventricle wall. Cardiac MRI presents a distinct picture depending on the pathology. Damage due to an ischemic insult or heart attack always extends from the subendocardium, which is the layer of the ventricle wall lining the cavity. Viral myocarditis extends from outside to inside, from the subepicardium to the midmyocardium. Trauma to the heart could also be subepicardial, but it will be accompanied by a little bleed in the ventricle wall. Both the left ventricle and right ventricle could be involved, with the former being the victim more often.
Remember, Commotio Cordis can occur with minimal trauma to the heart; hence, there may not be too much damage seen, such as avulsion of heart valves. Cardiac MRI, if done soon after the index event, could provide evidence of slight trauma and also rule out acute myocarditis or previous myocarditis that has left a residual scar. Late myocarditis, fibrosis, or scarring is detected by late gadolinium enhancement.
Enough of technicalities; the point I am raising is that to propose Hamlin is a clear-cut case of vax-induced myocarditis resulting in collapse is stretching it a bit too much. It is agreed that many young athletes have collapsed these past two years since the rollout of vaccines, and that many, if not most, of them are due to vaccine-induced myocarditis. But Hamlin’s may not be a vax-induced collapse. Circumstantial evidence favours Commotio Cordis; a cardiac MRI could have cleared the air. An endomyocardial biopsy soon after a traumatic injury may not have been the wisest course of action, but an MRI would certainly have been helpful. Crucially, cardiac MRI will not pick up every case of myocarditis or myocardial injury, and signs of fibrosis or scar tissue will not persist beyond 6 months in quite a few.
If myocarditis due to an mRNA vaccine or previous virus infection is strongly suspected or confirmed, an implantable cardioverter-defibrillator (ICD) becomes necessary to prevent a future catastrophe.