Cervical cancer, with 500,000 new cases each year, accompanied by 250,000 annual deaths, is not a disease to be trifled with. It happens to be the second most common cancer in women (1). Almost all cases of cancer of the cervix are due to infection with the human papillomavirus (HPV). The biggest culprits are HPV type 16 and 18. Two vaccines are available on sale against the HPV 16 and HPV 18, one of them is also effective against HPV 6 and HPV 11 , responsible for genital warts. The vaccine is administered as 3 intramuscular injections over 6 months(2-4). The human papillomavirus is sexually transmitted, which means females who have attained puberty are particularly susceptible. Persistence infection with HPV results in alterations of cervical epithelial cells after a period of 5 years. Around 10% of infected women go on to develop histological changes graded as cervical intraepithelial neoplasia (CIN 1), CIN 2 and CIN 3. The next grade is termed carcinoma in situ or CIS. The chances of developing full blown cervical are increased considerably once the cellular changes develop, but are still are as low as 1% to 10%, which means that a substantial number of females with precancerous cellular changes resolve spontaneously. Invasive cervical cancer arises over many years , peaking between 35 and 55 years of age (5). The HPV vaccine has no role once a person has become infected. Substantial reduction in HPV infection have been recorded, but effect on cervical cancer remains to be established due to the long lag time in development of invasive cancer subsequent to HPV infection. A systemic review of HPV vaccination of at least 50% in high income countries reported that HPV 16 and 18 infections significantly deceased by 68%, while anogenital warts decreased significantly by 61% in girls 13 to 19 years. Another recent meta analysis of observational studies on quadrivalent HPV vaccination has reported maximal reductions of approximately 90% for HPV 6/11/16/18 infection, approximately 90% for genital warts, approximately 45% for low grade cytological cervical abnormalities, over a 10 year period (6-8).
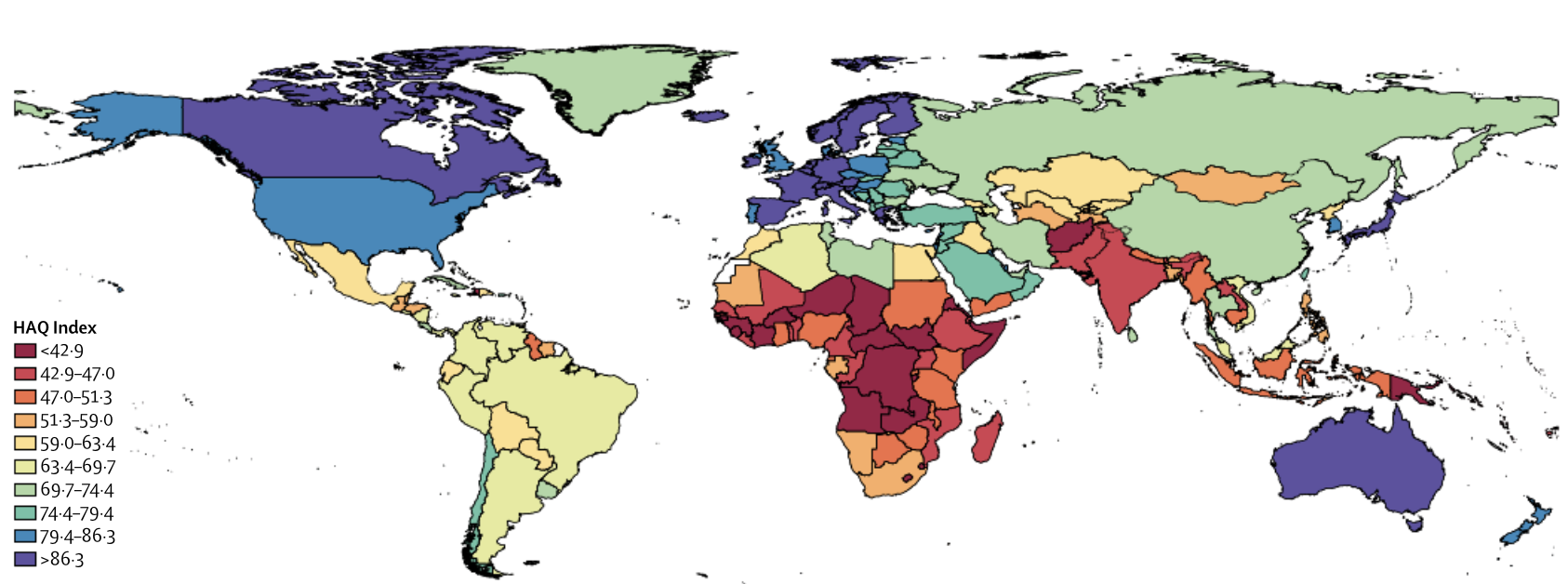
Cervical cancer is the second common cause of cancer mortality in women in India, with more than 122,000 new patients each year accompanied by almost 70,000 deaths.In fact 85% of cervical cancer cases are in low and middle income countries. Twenty five percent of cervical cancer deaths in the world occur in India. Despite the dire statistics the Ministry of Health and Family Welfare continues to mull over the decision to include the HPV vaccine in the national immunisation program. The reluctance of the government is largely because of a 2012 writ petition (public interest) filed against the vaccine in the Supreme Court, and political pressure by one of its own affiliates. With a single dose costing almost $ 50 in India, any Indian government would blanch at the idea of putting in billions of dollars on a single vaccine. The HPV vaccine is however available commercially in the private sector.
An excellent randomised study from India (9) reported that a single round of screening for HPV involving more than 130,000 women substantially reduced the incidence of advanced cervical cancer and cervical related mortality within 8 years. Screening therefore would be essential in women aged 25-40 years to manage pre cancerous cervical lesions and also cancer itself. A much earlier and probably the best intervention would be preventing infection by HPF; this is where a vaccine comes into play. We already have data demonstrating significant reduction in HPV infection by the vaccine.
Continue reading “HPV VACCINE SPLITS COCHRANE BOARD WIDE OPEN”