Primary percutaneous coronary intervention (PPCI) is the established technique for restoring flow in the infarction related blocked artery (IRA) in the setting of acute ST -segment elevation myocardial infarction (STEMI). Numerous randomized studies have confirmed that PPCI significantly reduced mortality, re-infarction and stroke as compared to thrombolytic treatment. What is however still not clear is what is to be done with the other coronary arteries if found blocked during PPCI; bearing in mind that approximately 30% to 40% of patients undergoing primary PCI for acute MI have multi but meta-analysis and observational studies have shown mixed results for complete revascularization. The guidelines had frowned upon tackling non-IRA in setting of STEMI and most physicians are reluctant to stent non-IRA because of the fear of complications and prolongation of the procedure. All professional cardiac societies recommend treating non-IRA only if hemodynamic compromise persists after opening up the IRA.
But now 2 randomized studies, albeit small and underpowered, have shown encouraging results with multi-vessel stenting in patients with STEMI during PPCI. The first paper (Preventive Angioplasty in Acute Myocardial Infarction or PRAMI) published in the NEJM reported significant lowering of adverse cardiac events with multi-vessel stenting compared to IRA stenting alone during PPCI in 465 patients of STEMI followed for almost 2 years. There was almost more than 65% reduction in cardiac death, non-fatal MI, and refractory angina with multi-vessel stenting versus IRA alone stenting. Bare metal stents were used in one third of patients in the multi-vessel group, almost 80% of patients in both groups received a glycoprotein 2b/3a inhibitor, all received dual anti platelet therapy for a year, and 90% of patients were on a beta blocker, ACE inhibitor/angiotensin receptor blocker and a statin. No stents were deployed in 5% of non-IRA in the multi vessel stenting cohort. The number of arteries treated in the MV stenting group were 1.4 and the mean diameter 3.1 mm. The authors concluded that there was substantial advantage in MV or preventive stenting (stenting the non-IRA artery) despite current guidelines not recommending such practice because of lack of evidence. This trial took 50% stenosis as cut off threshold to treat non-IRA. It is however still not clear whether the same approach can be applied equally successfully in patients with NSTEMI because of difficulty in define the IRA, and what should be the percentage block in the non IRA to be considered for intervention, whether a lesion less than 50% should be treated? The signs ant reduction in events in the PRAMI study cannot be simply explained by anatomical severity of block in the non-IRA. It is quite possible that a systematic inflammatory state exists in patients with STEMI that provides an environment for amplified thrombosis and endothelial dysfunction. This is the probable reason when one comes across patients of STEMI who have thrombi in a coronary artery other than the IRA and at times 2 vessels are totally occluded at the same time. The measurement of a physiologic block with fractional flow reserve (FFR) in non-IRA may not be predictive enough in the setting of STEMI, but this issue can only be resolved by a randomized study. The message from PRAMI is that non -IRA devoid of thrombi or significant block should not be presumed to be a healthy artery. It however remains to be solved whether preventive PCI should be done in the same setting or a few days later whilst the patient is still admitted in hospital.
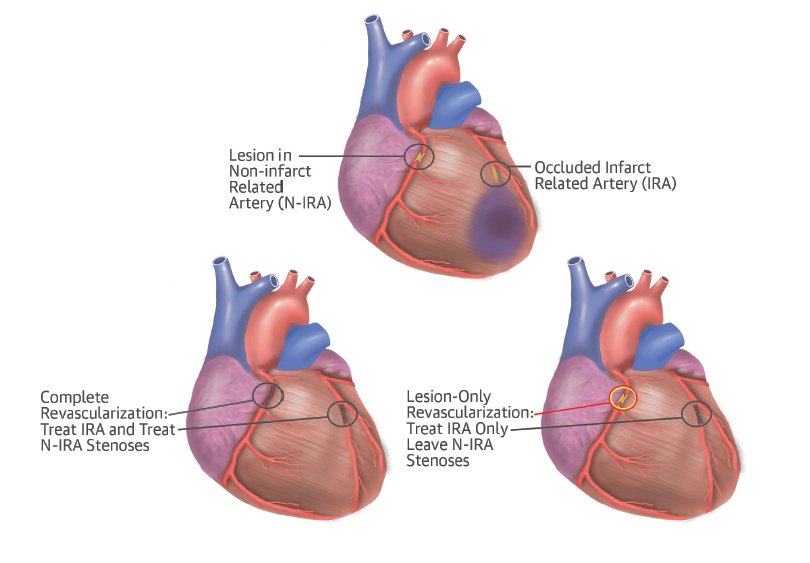
The second paper published in JACC called the CvLPRIT (Complete versus Lesion-Only Primary PCI Trial) trial (also from the UK) randomized almost 300 STEMI patients to complete revascularization or PCI of the IRA alone. The trial reported significant reduction in composite clinical endpoint of death, myocardial infarction, heart failure and ischemia driven revascularization. The primary outcome occurred in 10% of patients in the complete revascularization compared with 21% in the IRA alone treated group (hazard ratio 0.45; 95% confidence interval: 0.24 to 0.84); p=0.009) after a year. There was no increase in contrast induced nephropathy, major bleeding or stroke by complete intervention. Lesions selected for complete revascularization had to be at least 70% blocks or more than 50% stenosis in 2 separate views. Both PRAMI and CvLPRIT have shown in a randomized manner that complete revascularization is not only safe but actually improves clinical outcomes compared to IRA only PPCI. Larger randomized trials are needed to confirm these findings; the American College of Cardiology which had in 2012 recommended that only IRA be unblocked during STEMI, stated in September 2014 that “over the last 2 years new science has emerged showing potential improvement for some patients in their overall outcomes as a result of complete revascularization.” The 2 randomized studies mentioned above have altered the field providing evidence of improved outcomes with unblocking all major arteries in STEMI. The ACC however cautioned that a few questions remained un-answered “about the exact timing of the procedures; whether certain patients benefit versus others; whether fractional flow reserve might guide decisions; and the role of patient complexity and hemodynamic stability.” But formal changes in the guidelines as of now remain to be made.