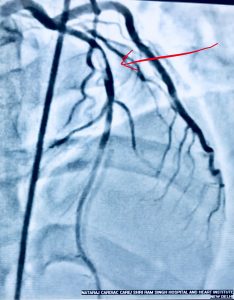
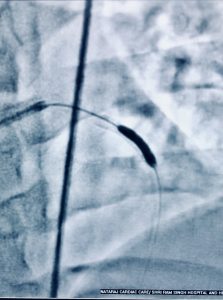
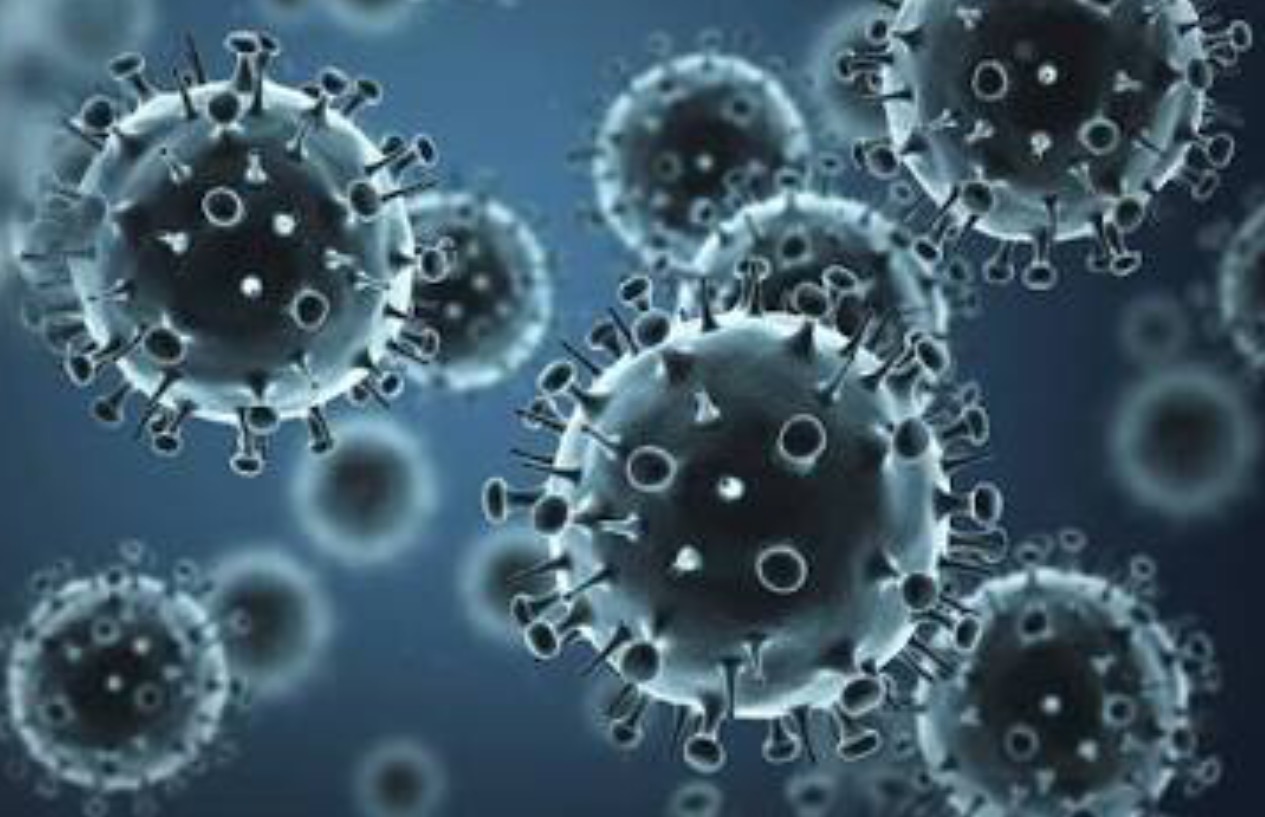
More than a decade ago a brilliant American marathoner form the United States collapsed and died 5 and a half miles into a marathon trial run for the Beijing Olympic Games. Ryan Shay was a world class long distance runner whose own Dad was a running coach. When Ryan was only 14 years old it had been noticed that his heart was a bit larger than most children, but this was ignored by everyone including his parents because he excelled in sports. Ryan had run numerous marathons before his death and was therefore presumed to be supremely fit. His death sent tectonic waves across the running world of north America. His legacy endures today with a prestigious annual mile race named after him. I had wondered aloud the on the cause of his death, and wrote so in the Times of India, Delhi edition then. I was afraid that maybe a drug had dome him in. The autopsy report was released more than 4 months after Ryan’s sad death. The report stated that Ryan did indeed have an enlarged heart but with dome scar tissue. It was surmised that viral myocarditis some time in the past accounted for the fibrosis in the young athletes heart. Ryan Shay died when only 28 years old. The normal electrical impulse of the heart is obstructed by fibrosis or scar tissue; it is rendered chaotic resulting in arrhythmia (irregular heart beat) ,which in turn can be fatal. The autopsy report of Ryan Shay concluded that fibrosis due previous viral myocarditis led to sudden cardiac arrest (SCA). There was no trace of hypertrophic cardiomyopathy in Ryan’s case, nor any evidence of a performance enhancer.
Most data on sudden cardiac arrest points out that the leading cause of death in young sportsmen is hypertrophic cardiomyopathy. Hypertrophic cardiomyopathy is a genetic disease (not rare) in which the heart muscle is thickened disproportionately in an erratic manner at the cellular level. The heart muscle cells are not arranged in an orderly fashion under the microscope, there is no brick by brisk pattern of a wall seen in hypertrophic cardiomyopathy. The cells are completely chaotic like an imaginary Van Gogh painting if drunk; this is the microscopic hallmark of hypertrophic cardiomyopathy apart from an obviously thickened heart , which can at times be asymmetric as well. The thickened heart muscle can be recognised on 2 D echocardiography by a reasonably trained doctor, or even a technician. One does not have to wait for a post mortem to confirm obstructive cardiomyopathy. But it should be remembered that elite athletes especially endurance athletes may have enlarged hearts too, accompanied by changes in the their ECG. An astute physician or cardiologist would be required to distinguish physiological heart enlargement from the pathological genetic one.
Continue reading “PRE-SCREENING SHOULD BE A MUST FOR YOUNG INDIAN ATHLETES”