The United States is currently in the grip of a flu epidemic with a100 people already reported dead. The flu vaccine seems largely ineffective and there is the grim probability of more mortality. The strain is the same as the “Aussie Flu” H3N2 that acts within hours. You could me normal in the morning and down by evening, have pneumonia the next day. Experts believe this is the same virus that killed more than 50 million people in the Spanish Flu epidemic of 1918. Mortality will definitely be much less this time around because of significantly improved medical care. Tamiflu however is running out of stock in the US. The same virus has decscended in the United Kingdom. England will be hit by an epidemic in a couple of weeks. Around 120 people have already died in the U.K, where predominantly the culprit strain is influenza B ( B Yamagata or the Japanese Flu). The trivalent flu vaccine is ineffective against Japanese flu.The developing furore over lack of efficacy of the vaccine is likely to submerge findings of 2 recent trials that suggest clopidogrel may be as effective as ticagrelor despite guidelines recommending that ticagrelor or prasugrel combined with aspirin be preferred to clopidogrel plus aspirin for at least a year subsequent to a percutaneous coronary intervention (PCI) in patients of acute coronary syndrome ( ACS). Both ticagrelor and prasugrel are more powerful anti platelet agents albeit associated with significantly greater bleeding.
The TOPIC trial randomised 646 ACS patients to ticagrelor or prasugrel plus aspirin ( 323 patients)and after one month to clopidogrel plus aspirin (323 patients) post PCI. More than 90 % received a drug eluding stent and almost all patients were treated by the radial route. After one year the patients who were switched to clopidogrel plus aspirin had more than 50% reduction in the combined clinical end point of death, urgent revascularisation, stroke or bleed ( from 26% to 13%). There was no difference in ischemic events (11.5% versus 9.3%), while bleeding was substantially more in patients assigned to ticagrelor or prasugrel plus aspirin as compared to clopidogrel plus aspirin (15% versus 4%). The researchers explained their findings by the clinical observation that stent thrombosis is commoner in the first few weeks and months and that as time passes bleeding becomes a greater concern with ticagrelor or prasugrel. Switching to clopidogrel with aspirin after the first 4 weeks seems a reasonable clinical option as ischemic events are equivalent with the bonus of reduced bleeds.
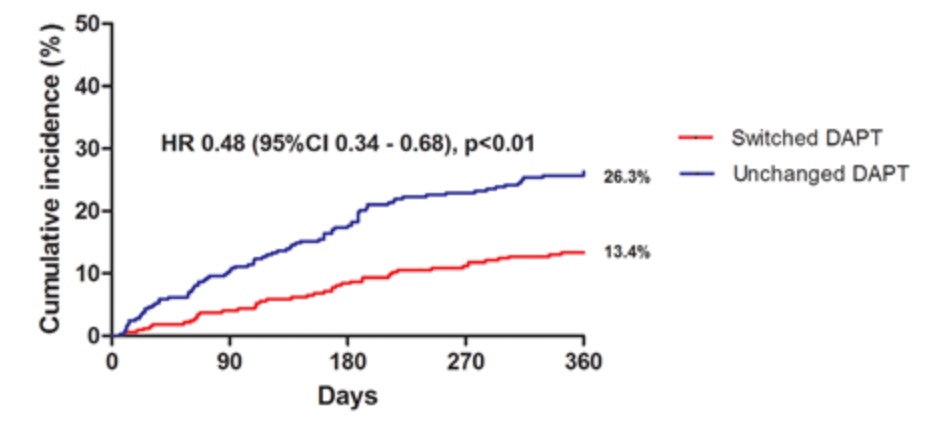
Patients in TOPIC had a mean age of 60 years, 80% were males and 40% had ST elevation myocardial infarction.
The TOPIC study may not go down very well with the industry but should provide adequate food for thought for clinicians. The TOPIC trial is undoubtedly too small to modify guidelines but could launch a larger trial assessing difference in efficacy and safety in switching to the more economical clopidogrel from ticagrelor one month post PCI. It is a different matter that one clinicians may be already following such an approach.
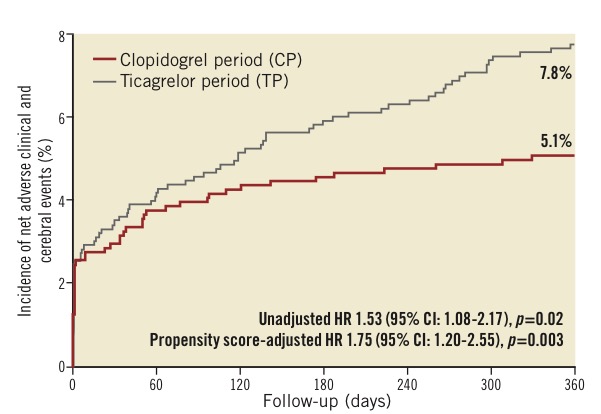
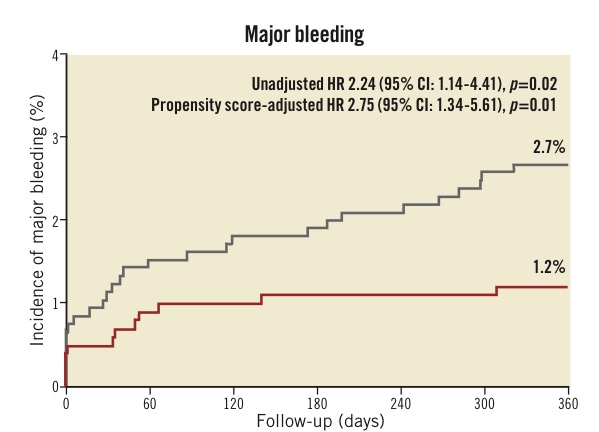
The other study of note is an observational trial test compared a thousand patients who had been on clopidogrel to a cohort of another thousand patients on ticagrelor. This trial was called the CHANGE DAPT study that was reported at the European society of cardiology 2017 meeting. Bleeding complications were halved with clopidogrel as compared to ticagrelor,while there was no significant difference in ischemic events. The CHANGE DAPT trial provided contrary results to the much larger PLATO trial ( which was also randomised). PLATO had reported superior ischemic results with ticagrelor as compared to clopidogrel in patients with acute coronary syndrome.However only 65% patents underwent PCI and 60% patients had implantation of bare metal stents in PLATO. The remaining patients got earlier generation DES. The primary end point of death, stroke, or major bleeding, which was reduced from 8% in the ticagrelor era to 5% in the clopidogrel era. The difference was mainly driven by reduction in bleeds. The higher rate of bleeds in the ticagrelor era was observed despite greater use radial approach, more administration of proton pump inhibitors and lesser use of GP IIB/3A inhibitors. The increase in bleeding with ticagrelor is yet to be explained beyond the fact that is a very potent anti platelet drug.
How on earth did clopidogrel trump ticagrelor in an observational study ? One explanation is the greater use of newer generation drug eluting stents that have extremely thin struts. The CHANGE DAPT trial compared clinical results in patients who got clopidogrel (2012-2014) to patients who received ticagrelor (2014-2015). The composite end point of death, myocardial infarction or stroke was no different but bleeds were substantially lower with clopidogrel. Both TOPIC and CHANGE DAPT provide some provocative albeit hypothesis generating results. A large randomised trial ( GLOBAL LEADERS) has included 16000 patients who will undergo PCI; following PCI , patients of one group at 30 days will receive ticagrelor alone while the other cohort shall continue with ticagrelor plus aspirin.
Randomised trials undoubtedly provide the most scientifically robust data but there is a chink in the armour. Patients in randomised trials do not always represent real world patients, also they get more personal treatment. The SWEDEHEART registry that included 45,000 patients did report better results with ticagrelor, but patients who received ticagrelor were at lower risk of death or bleeds.
Results of the PLATO trial this had BMS inserted in almost two thirds of patients may not be applicable with ultra thin DES used in contemporary practice. The advantage of reducing ischemic events with ticagrelor may be lost with newer generation DES, while bleeding complications seem to linger on. The clinical implications are that treatment should be individualised with emphasis on ischemic and bleeding vulnerability of the patient.
In a middle income country like India the role of the relatively weak anti platelet agent such as clopidogrel cannot be dismissed in patients of ACS undergoing PCI.