
The Takotsubo syndrome (TTS) is an acute heart failure syndrome that largely affects post-menopausal women. It was (first) described by the Japanese in 1990; the disease is defined by transient systolic and diastolic left ventricle dysfunction accompanied by a range of wall motion abnormalities. It predominantly affects elderly women and is usually preceded an emotional or physical trigger. It is accompanied by substantially increased morbidity and mortality that equal those of acute coronary syndrome (ACS). The clinical presentation in the acute phase consisting of electrocardiographic findings and biomarker profiles are not dissimilar from ACS. In fact 1% to 2% of suspect6ed patients of ACS are actually suffering from TTS. Both TTS and ACS have many common clinical features at admission.
Takotsubo syndrome, for many years has been believed to be sparked predominantly by an emotional trigger. It has been recently recognized that physical triggers too can trigger TTS, and at times there may be no triggers at all. The exact pathophysiological mechanism triggering TTS however still remains unclear. The role of a brain-heart axis in the pathogenesis of the syndrome has been well recognized. Various psychological and physical conditions have been documented as triggering factors for TTS.
Emotional problems range from sudden accidents (witnessing a husband get severe burns in a house-fire, seeing a grandson’s traffic accident, sudden death of husband, attending funeral of a relative, anxiety over a congenital condition problem in family member, quarreling and watching TV. Physical triggers have been reported as acute phase cerebrovascular accident, epileptic fit, exacerbation of asthma, commencement of dialysis therapy, acute abdomen with pain, during a procedure (intubation, tracheotomy, trans bronchial lung biopsy, delivery, cholecystectomy, and colectomy).
The Journal of American College of Cardiology recently published data from 505 of TTs form a Swedish register. This report compared patients of TTS to 2 groups: 1) patients of ACS (unstable angina or STEMI treated with PCI) and the other group 2) patients with chest pain of unknown cause and non-obstructive coronary arteries. The main finding of the study was that adjusted long-term mortality of TTS is similar is similar to patients with ACS but much worse than patients of chest pain with normal coronaries. The conclusion drawn is that prognosis in TTS should never been underestimated, and is as grim as that of patients admitted for ACS.
Takotsubo syndrome patients can be divided as a “primary” or as a “bystander” disease in patients admitted for other reasons. “Bystander” TTS patients have a worse prognosis because they carry co-existing disease. The pathogenesis of TTS remains elusive despite a quarter century of investigation. The initial explanation was vasospasm but the wall motion abnormalities of left ventricle do not correspond to the concerned coronary artery. The Swedish registry data reveals that 95% of patients of TTS did not suffer from migraine and that 98% patients were not taking anti-migraine drugs. Migraine is associated with vasospasm, and hence the Swedish data goes against the theory of spam as a cause of TTS. The theory of coronary artery pathology remains speculative because left ventricle wall damage observed in TTS just does not follow coronary artery territory.
The other idea proposed in pathogenesis of TTs is that of stress, catecholamines and the autonomic nervous system. However, unequivocal evidence of cause and effect is lacking. Many patients develop TTS by a stressful trigger, but 30% of patients develop TTS without any known trigger.
Beta-blockers can be life saving during the acute phase of TTS and could be life saving in patients with left ventricular obstruction with apical TTS. There is no data on long-term administration of beta-blockers for secondary prevention in patients with TTS. The fact that almost 50% of patients with recurrent TTS are on beta-blockers suggests little value of the drug for secondary prevention.
The International Takotsubo Registry including 26 centers in Europe and the US reported that of 1750 patients of TTS, 90% were women (mean age, 67 years). Emotional triggers were less than physical triggers (28% vs. 36%) and 29% patients had no trigger. More patients with TTS as compared to patients of ACs had neurologic or psychiatric disorders (56% vs. 26%) and mean left ventricle ejection fraction was significantly lower (41% vs. 52%). Rates of shock and death were similar in the 2 groups. During long tern follow-up, the rates of cardiac events were 10% per patient-year, and the rate of death was 6% per patient-year. The Registry published by the NEJM in 2015 concluded that TTS represents an acute heart failure syndrome with substantial morbidity and mortality. Apical TTS was seen in 82% of patients, the mid ventricle variety was found in 15%, and basal and focal forms were diagnosed in 2.2% and 1,5% respectively.
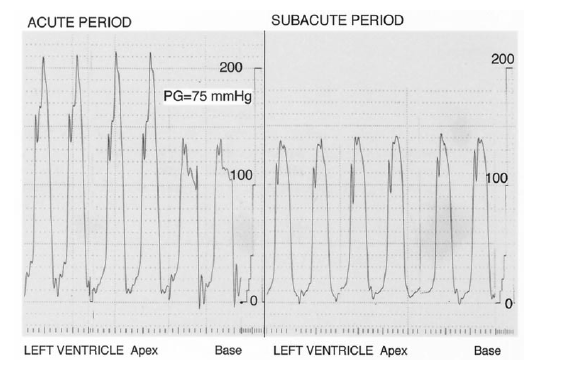
Several mechanisms have been proposed to explain apical ballooning in TTS; 1) the LV apex does not have a 3-layered myocardial structure, 2) easy loss of elasticity post expansion of the apex, 3) the LV apex is the border zone for perfusion by coronary arteries. The prevalence of dynamic left ventricular outflow obstruction (LVOTO) varies from 10% to 20% of patients, but treatment strategies remain uncertain apart from administration of beta-blockers. No randomized clinical trial has studied pharmacological treatment strategies in patients with TTS. Inotropes are contraindicated because a large body of preclinical and clinical evidence implicates catecholamines in the pathophysiology of TTS. Crucially, it cannot be over emphasized that myocarditis has to be ruled out in patients presenting with the focal variety of TTS. Myocarditis can be ruled out with endomyocardial biopsy or cardiac magnetic resonance imaging (MRI). Takotsubo cardiomyopathy presents with myocardial edema minus delayed enhancement, on MRI.
It is obvious that prospective large studies are conducted to confirm the exact pathogenic factors causing TTS and the best short-term and long –term treatment options.