A significant number of patients undergoing PCI with stenting are also suffering from atrial fibrillation (AF). These patients need triple antithrombotic therapy in the form aspirin plus clopidogrel (or another P2Y12 inhibitor) and an oral anticoagulant such as warfarin. Triple therapy is aimed at reduction of emboli (systemic or cerebral), ischemic events (myocardial infarction, death, stroke) and stent thrombosis. Triple antithrombotic therapy is however used with the caveat that there is a substantial increase in fatal and not fatal major bleeding. An alternative strategy is emerging that employs dual antithrombotic therapy of dabigatran (direct thrombin inhibitor) and a P2Y12 inhibitor (clopidogrel or ticagrelor) to prevent thrombotic events without increasing the risk of major bleeding. Aspirin is not included in this prescription. In the multicenter RE-DUAL PCI trial more than 2700 patients with non valvular AF were randomly divided to receive dabigatran 110 mg or 150 mg twice a day with a P2Y12 inhibitor (clopidogrel or ticagrelor) or triple therapy (warfarin plus aspirin plus a P2Y12 inhibitor). These patients had undergone PCI and stenting in the previous 120 hours. The primary endpoint of time to major or clinically relevant non-major bleeds was significantly less in the dual antithrombotic group (hazard ratio 0.52; p<0.01 for non inferiority). At 14 months major bleeds were 15% in the dabigatran 110 mg (twice day) plus P2Y12 inhibitor group versus 27% in the triple antithrombotic group), an absolute difference of 12%. Major bleeds were also significantly lower in the 150 mg dabigatran dual therapy group compared with triple warfarin therapy group. There was no difference in thromboembolic events and deaths in dual versus triple antithrombotic groups, indicating similar efficacy regarding ischemic events. The researchers conclude that in patients with AF undergoing PCI with stenting, a regimen of dabigatran with a P2Y12 inhibitor dual therapy significantly slashes the risk of major bleeds as compared to warfarin triple therapy, with no increase in thrombotic complications.
It is known that almost 1 in 4 patients (>65 years in age) of AF undergoing PCI are discharged on triple therapy. Those getting triple therapy have higher rates of major bleeds versus those on dual antiplatelet therapy (DAPT) alone, without any measurable difference in composite of myocardial infarction, death, or stroke. There is also the clear danger of increased intracranial bleeding.
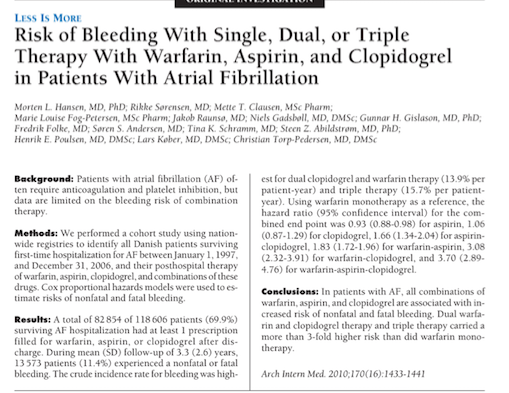
Many patients with AF require long-term anticoagulation with a vitamin K antagonist. Patients with AF may also have coronary artery disease requiring treatment with PCI and stenting. Numerous previous trials have reported increased risk of major bleeding when warfarin is added to dual antiplatelet treatment. The risk of fatal or non-fatal bleed is raised 4 folds compared to warfarin alone, while risk of intracranial hemorrhage goes up twice when compared to DAPT alone. Moreover shortening the course of triple therapy does not reduce risk of major bleeds.
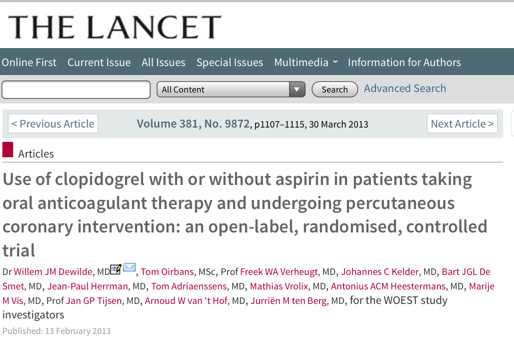
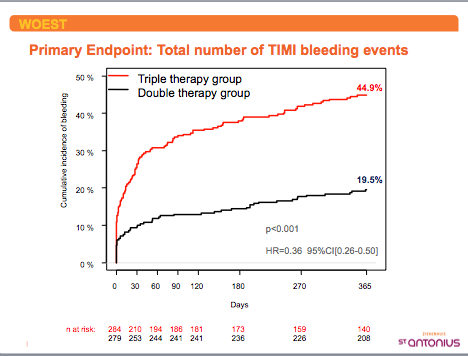
The WOEST trial included almost 70% of patients with AF. Those patients assigned to warfarin and clopidogrel versus triple therapy had significantly lower rates of major bleeds without any risk of increased thrombotic events. Patients in the WOEST trial were treated with warfarin and clopidogrel. The WOEST investigators proposed that a strategy of warfarin plus clopidogrel, but without aspirin could be applied in patients on oral anticoagulation when undergoing PCI.
In the PIONEER AF-PCI trial, more than 2000 patients were randomly assigned, in a 1:1:1 ratio of 3 groups, low dose rivaroxaban (15 mg daily) plus a P2Y12 inhibitor, very low dose rivaroxaban ( 2.5 mg twice a day ) plus aspirin and a P2Y12 inhibitor, and a third group that got warfarin triple therapy. The investigators reported significantly lower rates of significant clinical bleeding in the low dose warfarin plus P2Y12 inhibitor group and also the very low dose rivaroxaban plus aspirin with P2Y12 inhibitor cohort versus warfarin triple therapy group. The PIONEER AF-PCI trial was not powered to pick up differences in ischemic events, however there were no excess ischemic events noted with dual treatment.
A meta analysis of these three trials including AF patients undergoing PCI has revealed that major and minor bleeds with dual therapy are cut down by half as compared to triple warfarin treatment. The risk of death, myocardial infarction, revascularization, stent thrombosis, or thromboembolic events was not found to be higher with dual therapy. Hence for now the take home message is dual treatment should be favored against triple warfarin therapy in AF patients subjected to PCI. The best combination however needs to be established. It may be years before we can be sure whether rivaroxaban plus clopidogrel is more effective than rivaroxaban plus ticagrelor, and whether dabigatran plus clopidogrel is superior to dabigatran plus ticagrelor. A head to head comparison of rivaroxaban (or another X a inhibitor) with dabigatran would also make for exciting research.
The average age of patients (in the RE DUAL PCI trial) was 72 years, two thirds were males, more than a third had diabetes and about 25% had previous MI. More than half of patients suffered from acute coronary syndrome. Drug eluting stents were deployed in more than 80% while almost 15% patients had a bare metal stent implanted.