Percutaneous coronary intervention has rapidly evolved in the last 38 years from the the first from percutaneous balloon angioplasty (BA) done in 1977, insertion of bare metal stents (BMS) in the eighties, to deployment of metallic drug eluting stents (DES) since 2000. It was realized in the eighties that coronary stents were mandatory in most cases of PCI to prevent catastrophic coronary artery recoil following BA, to tack up dissection, and to reduce restenosis. Second generation DES with much finer struts have now become the norm because they reduce restenosis and stent thrombosis in stable angina and acute coronary syndrome patients as compared to earlier DES and BMS. All second generation DES however still carry the risk of chronic inflammation by the polymer that holds and elutes the drug, and the phenomenon of late neoatheroslerosis. The metallic stent moreover jails the concerned artery preventing vascular reactivity and blunting coronary dilation and constriction; they can also block a significant side branch if inserted at a bifurcation. These potential disadvantages led to hectic research on a fully bioresorbable scaffold capable of melting away in 2-3 years.
It is now established by pathological specimens on autopsy, and intra-coronary imaging by intra-vascular ultrasound (IVUS) or optical coherenence tomography (OCT) , that late stent thrombosis (> 1 month after index procedure) and very late stent thrombosis ( > 1 year after PCI) albeit uncommon, but having fatal ramifications, are due to persistent inflammation or incomplete endotheliazation of metallic stent struts. The polymer jacket over the struts is pro-inflammatory and elicits eosinophilic reaction in the arterial wall.
The fully bioresorbable scaffold (BRS) provides the spectacular promises of disappearing in 2-3 years, and thereby releasing the vessel from it’s metal jacket; recovery of the coronary artery to dilate; and permitting easier imaging with CT coronary angiography or MRI.
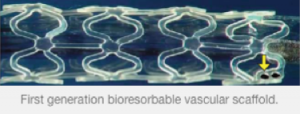
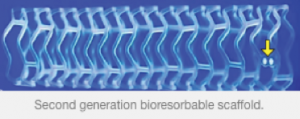
Currently 16 different scaffolds are at different stages of development and 2 have already been CE mark approved for clinical use. There are 2 Indian companies also in the process of developing BRS. The Abbot everolimus drug eluting poly-L-lactic acid (PLLA) backbone based BRS has so far been most studied in human trials. The coating storing the drug (everolimus) to be released is also resorbable and made up of poly D,L-lactic acid ( PDLLA).
The first study ( ABSORB Cohort A)was done on 30 stable angina patients with discrete lesions; 3X12 mm and 3X18 mm BRS were used in this study, which revealed that albeit the device was feasible to use, there was evidence of acute recoil with significant late luminal loss or narrowing at 6 months. This compelled the company to come out with an improved design by increasing radial strength and improving deliverability. The strut size remained 150 um. and PLLA was persisted as the backbone. The next study ( ABSORB cohort B) demonstrated reduced recoil and late luminal loss. Major adverse cardiac events (MACE) at 2 years follow-up were only 8% (3 non ST-segment elevation myocardial infarction, and 6 ischemia driven target vessel revascularization). The lumen area was found to increase at 2 years (by IVUS) from 6.5 square mm to almost 6.9 square mm. Vascular reactivity had recovered by 12 months. The PLLA backbone had radial strength comparable to a metallic stent and was about 1200 mm Hg at implant, and 800 mm Hg at the end of a year. This PLLA backbone degrades to lactic acid by hydrolysis, which is then converted by the Krebs cycle into carbon dioxide and water.
The ABSORB EXTENT trial studied 250 patients with small and long coronary arteries; the MACE rate at 2 years follow-up was 7.3% and stent thrombosis only 0.8%. The ABSORB II randomized trial comparing BRS with the second generation Xience DES in 501 patients noted at the end of one year similar acute recoil but lower incidence of worsening or new angina in the BRS group of patients (22% vs 30%; p=.04). Three patients with BRS had stent thrombosis versus none in DES; more myocardial infarction in BRS (4% vs 1%) while there was more target vessel revascularization (TLR) with DES (2% vs 1%). The difference in composite of death, myocardial infarction and TLR was insignificant (5% and 3% in BRS and DES cohorts). Clinical outcomes in these trials have encouraged operators to insert more than 60,000 BRS in the last 3 years.
The other CE approved commercially available scaffold is the DESolve scaffold; which is also made from PLLA and releases a mixture of anti-inflammatary myolimus and PLLA, has strut thickness of 150 um, and is resorbed in approximately a year.
Salutatory clinical outcomes have been reported with BRS in patients with STEMI, a clinical situation where it would obviously be difficult to deploy the right sized scaffold to prevent complications during and post procedure. The scaffold was successfully inserted in 41 patients of STEMI in the ‘Prague 19’ trial. An OCT sub-study demonstrated excellent procedural deployment with good apposition; TIMI 3 flow was restored in 95% of patients. The authors concluded that BRS was feasible, safe and effective in STEMI. The BRS has also been found to be effective in diabetic patients.
The Abbot BRS device comes in 3 lengths of 12 mm, 18 mm, 28 mm; and in 3 sizes of 2.5 mm, 3 mm and 3.5 mm. There are anecdotal reports of successful deployment of these devices in chronic total occlusions, bifurcation lesions and left main blocks. They have also been used for treatment of saphenous vein graft and left internal mammary artery stenosis. The manufacturer strongly advises that the scaffold balloon is inflated gradually over 1 minute; around 1 atmosphere over 5 seconds. It is imperative that the lesion is prepared well by pre-dialatation with a non-compliant balloon of the same size as the vessel diameter, and subsequent to post deployment of the scaffold another non-compliant balloon is inflated to 18-22 atmospheres to ensure optimal expansion of the struts of the scaffold. The BRS has also been used for in-stent restenosis.
In the event of dissection or compromise of the side vessel during bifurcation PCI it is recommended that the struts against the side branch are sequentially opened by non-compliant balloons up to the size of the side branch diameter. Then another BRS is inserted with the proximal platinum marker covering the ostium of the side branch ( and a trifle inside the main branch) at 12-14 atmospheres. Next a ‘’mini-kiss or a ‘snuggle’ should be done with the side branch balloon proximal end adjacent to the main branch balloon.
The BRS should never be expanded more than the manufactured size to avoid distortion and breakage of the struts. The maximal expansion beyond the recommended diameter size is 0.1-0.2 mm which is obtained by post scaffold deployment optimization with a non-compliant balloon at 18-22 atmospheres.
A recent registry noted that stent thrombosis rates were higher with BRS than second generation DES; stent thrombosis was 1.5% at 30 days and 2.1% at 6 months. Most occurred in the first 30 days while 87% of patients were still on dual antiplatelet therapy. It is to be noted that this was not a randomized trial and it is quite probable that lesion preparation or post scaffold optimization was not rigorous enough.
The bottom line is that a if a 50-55 year old man with a heart attack (the usual presentation in India) is given a choice after informed consent , he may prefer the fully bio-absorbable scaffold to a DES, because the former would not stay permanently fixed in his coronary artery , for the rest of his life, eradicating lingering problems that accompany a DES.