Dr. Deepak Natarajan
Director Interventional Cardiology
MBBS,MD,DM
DELHI, NCR

A CASE OF PROSTHETIC VALVE THROMBOSIS
PCI IN DEXTROCARDIA SITUS INVERSUS AND SEVERE HYPO
Acute ST-Elevation Myocardial Infarction Triggered
UNPROTECTED LEFT MAIN OSTIAL AND SHAFT PCI IN A PATIENT WITH IMPENDING STEMI
By Deepak Natarajan
Tuesday, February 19, 2013
Operator(s):
Deepak Natarajan, Nirmalya Mukherjee and Rohit Kumar.
Affiliation:
Cardiological Society of India.
Facility:
Moolchand MedCity, New Delhi, India
History:
A 56 year male who had been smoking for more than 4 decades and had undergone PCI with stenting of his mid left anterior descending (LAD) artery in 2004 presented with severe retrosternal chest pain with perspiration and breathlessness. His 12 lead ECG revealed sinus rhythm with ST elevation from V1-V3 and ST segment depression in L2, L3, and AVF (Figure 1). The patient had persisted with smoking and had been erratic with his medication.
Angiography:
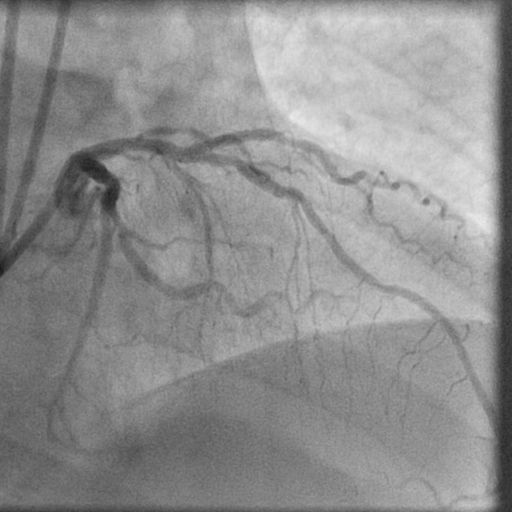
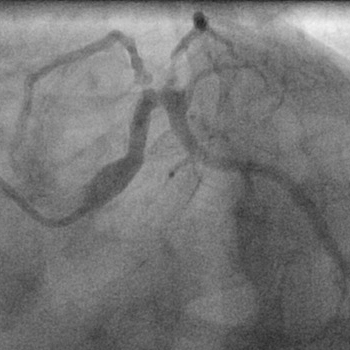
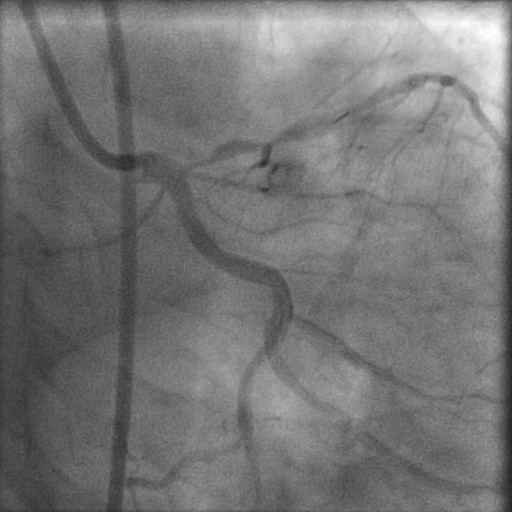
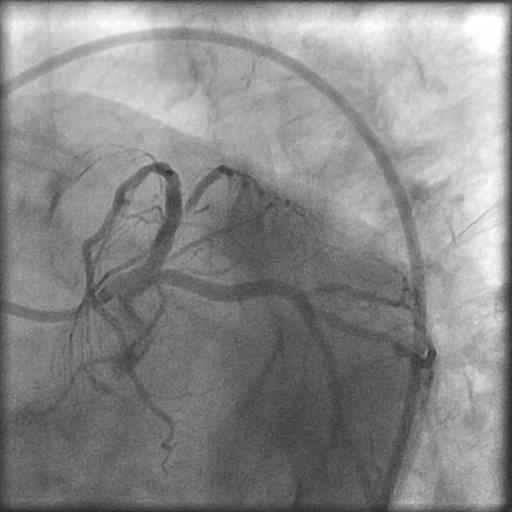
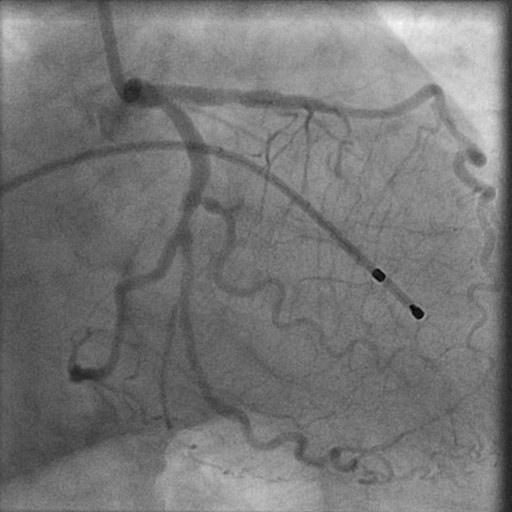
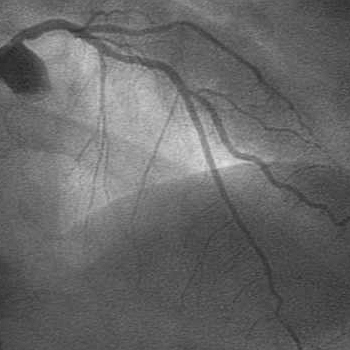
1) RCA: Near normal and dominant and providing collaterals to the left circumflex artery (LCX) (figure 2).
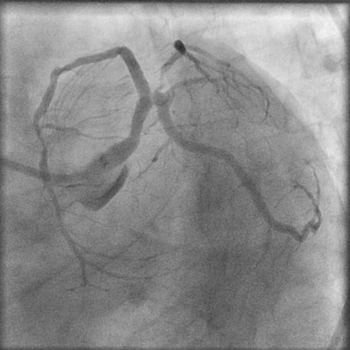
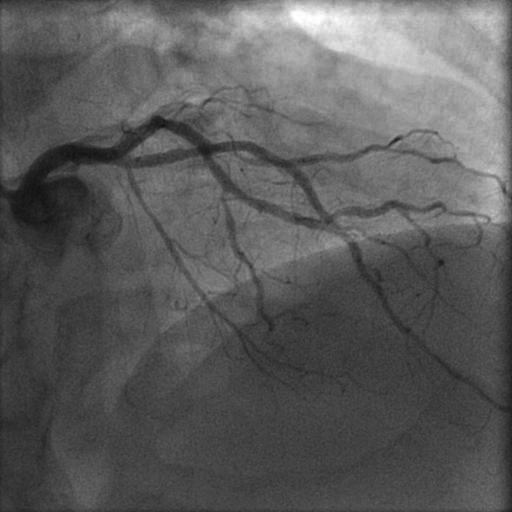
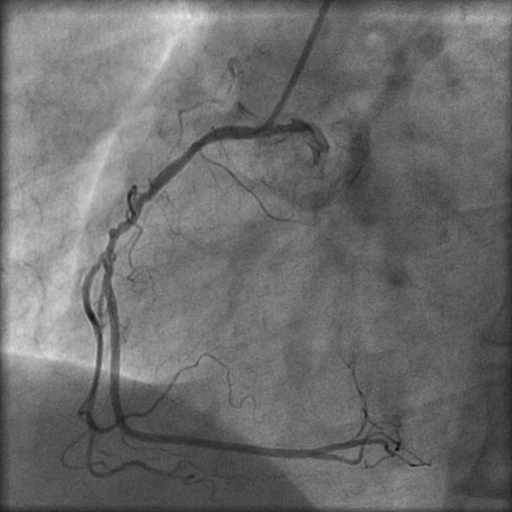
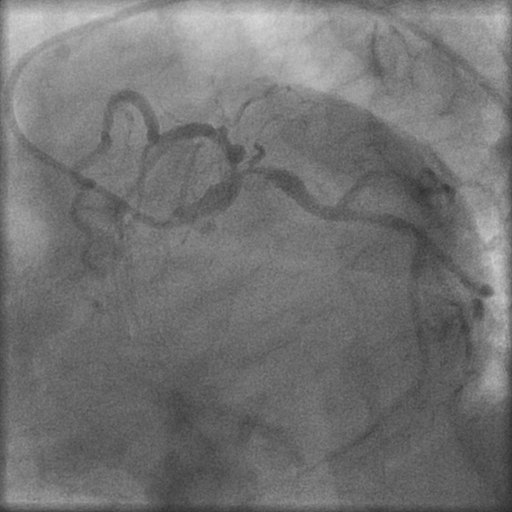
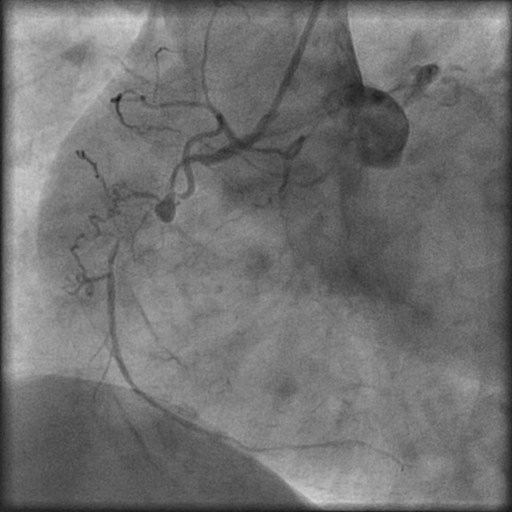
2) LM: 85% ostial stenosis with a 50% stenosis of the proximal LAD. The stent in the LAD was patent. The LCX was totally occluded proximally (figure 3, figure 4 ).
3) The SYNTAX score was calculated at 30 (intermediate risk group).
Procedure:
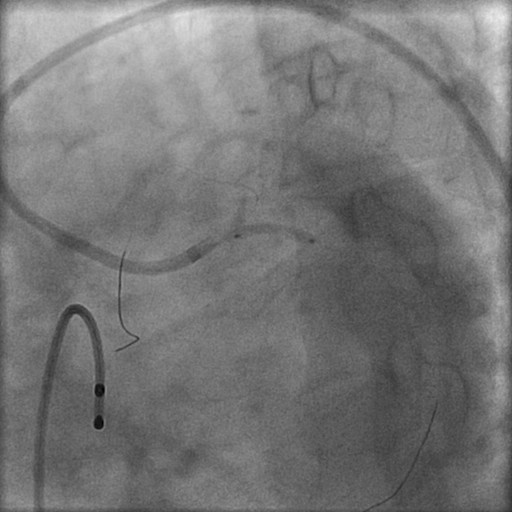
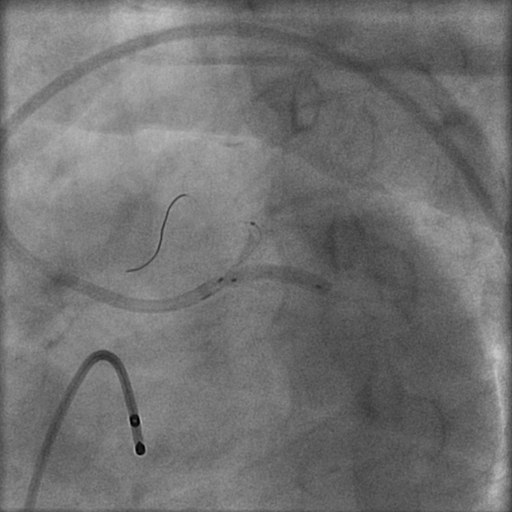
In view of the acute coronary syndrome setting it was decided to do PCI of the left main lesions. A 0.014″ floppy guidewire was negotiated across the LM lesions into the LAD. The LM lesions were pre-dilated with a 2.5x15mm balloon (figure 5) with the balloon protruding slightly into the aorta. A 3.5x15mm Resolute DES was similarly positioned with slight extension into the aorta and deployed at 16atm (figure 6, figure 7). Post-dilation was performed with a 4.5X12mm NC balloon at 18atm (figure 8).
Conclusion:
Angiogram demonstrated brisk TIMI 3 flow with no residual stenosis (figure 9, figure 10). There was also rapid resolution in his 12 lead ECG (figure 11).
Comments:
Significant unprotected left main coronary artery stenoses occur in 5-6% of patients undergoing coronary angiography. Meta-analyses have shown similar mortality rates up to one year with CABG and PCI, but repeat revascularization has always been more common with PCI while CVA has always been greater with CABG.
The 5-year results of the SYNTAX trial has showed comparable mortality and myocardial infarction rates in patients with LM disease undergoing CABG and PCI in the low and intermediate SYNTAX score groups. The results were quite different in patients with 3-vessel disease where CABG was superior in the intermediate and high SYNTAX score groups.
This patient had an intermediate risk (SYNTAX) score with lesions of his left main ostium and shaft. Left main disease of the ostium and or body are considered a 2a indication by both European and American interventional cardiology societies. But this patient also had multivessel disease and would therefore fall in the 2b indication slot. Managing ostial/shaft left main disease is relatively simpler than distal left main disease, but care must be taken to ensure that the stent protrudes just a little bit proximally into the aorta. In this case a second generation DES was utilized; it may perform the same or better than the paclitaxel DES used in SYNTAX. The ongoing EXCEL trial compares Xience (everolimus eluting) stents with CABG in patients with left main disease.
In the ACS setting PCI for ULMCA carries an in-hospital mortality rate of almost 20% while death rates have been found to be about 11% in patients with ST-segment elevation myocardial infarction.
Conflict of Interest:
None
MASSIVE CORONARY AIR EMBOLISM DURING PRIMARY PCI FOR ACUTE INFERIOR STEMI
By Deepak Natarajan
Monday, November 28, 2011
Operator(s):
Deepak Natarajan, Mafooza Rashid, Betshiba Dinaker, Vijeta Maheshwari, Nirmalya Mukherjee.
Affiliation:
Cardiological Society of India.
Facility:
Department of Interventional Cardiology
Moolchand MedCity, New Delhi, India
History:
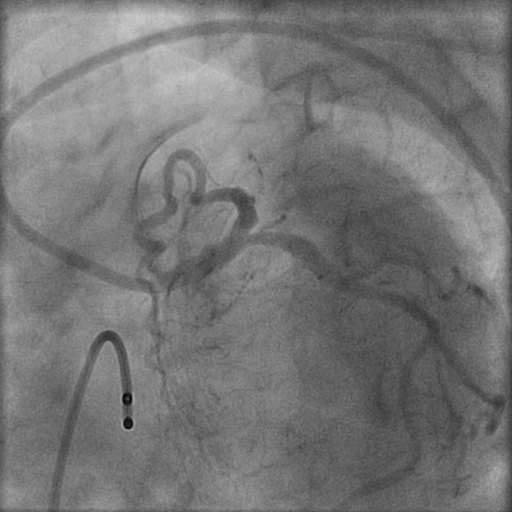
A 52 year male who was a chronic smoker was admitted for severe crushing retrosternal chest pain accompanied by nausea and perspiration for the previous 4 hours. He had no previous history of hypertension or diabetes. On examination in the ER he had a heart rate of 62-66 per minute, blood pressure 130/76 mm Hg, a fourth heart sound on auscultation, but no cardiac murmur. His chest was clear. His ECG revealed an acute infero-lateral myocardial infarction (Figure 1).The patient was given 325 mg aspirin, 600 mg clopidogrel and 5000 units heparin.
Angiography:
1) LAD: Normal
2) LCX: 80% stenosis proximally (figure 2).
3) RCA: 100% mid occlusion (figure 3)
Procedure:
The RCA was engaged with a JR 6Fr guiding catheter, and a 0.014″ floppy guidewire was used to cross the occlusion. After pre-dilation with a 2×10 mm balloon and intracoronary administration of 25 mcg/Kg of tirofiban, a 2.75x18mm bare metal stent was deployed at 16 atm with excellent antegrade flow and no residual stenosis (figure 4). The patient, however, continued to be restless and in pain. It was decided therefore to tackle the LCX lesion in the same sitting. The left coronary artery was engaged with a 6 Fr EBU guiding catheter, the same floppy guidewire used for the RCA intervention was positioned in the distal LCX, and the LCX lesion was predilated using a 2x12mm balloon(figure 5). Because the result was not satisfactory, 2.5x10mm balloon was introduced into the guiding catheter over the floppy guidewire. It was suddenly observed that the pressure wave was getting damped, and the systemic pressure was rapidly dropping (figure 6). Angiography demonstrated massive air embolism in both LAD and LCX arteries with no contrast flow beyond the mid segments of both arteries (figure 7). The patient was pulseless with electromechanical dissociation (figure 8). The balloon that was still in the guiding catheter was rapidly removed, and an attempt was made to suck out the air from the left coronary arteries via the guiding catheter. There was absolutely no improvement. Therefore, the guiding catheter was disengaged, and cardiopulmonary resuscitation (CPR) initiated with vigorous external cardiac massage (figure 9, figure 10). The patient was given 100% oxygen.The patient by now had received 2 IV atropine injections and was also put on IV dopamine. External cardiac massage was maintained for almost 4 minutes by which time the patient recovered both his heart rate and blood pressure. After ascertaining that the patient was hemodynamically stable (figure 11) and had fully recovered his consciousness, the LCX was stented with a 3x18mm sirolimus eluting stent at 14atm. (figure 12) with TIMI 3 flow and no residual stenosis (figure 13).
Conclusion:
The patient was asymptomatic by the time he was moved to the coronary care unit, and his ECG showed almost complete resolution of the elevated ST segments seen prior to the procedure (figure 14). The patient was discharged after 48 hours.
Comments:
Coronary air embolism, albeit rare (incidence ranging from 0.2%- 0.8% during percutaneous interventions) can have a heterogenous presentation ranging from mild symptoms to cardiac arrest and death. Air can be introduced inadvertently by inadequate aspiration of the guiding catheters, rupture of balloons, and leakage of air via a defective manifold system. The management of massive air embolism as seen in this case has to be extremely quick with 100% administration of oxygen to drive out the nitrogen from the air bubbles along with supportive measures such as CPR with emphasis on external cardiac massage. Aspiration and also forceful injection of contrast has been recommended. Aspiration did not work in this case, and forceful injections or manipulation of the guidewire were avoided because of the fear of traumatizing the left main, LAD, or LCX arteries. Aspiration with the Export catheter has also been described in a case report. Coronary air embolism during coronary angiography or PCI should be prevented by careful emphasis on good techniques during the procedure. Treatment has to be rapid and should consist of 100% oxygen accompanied by CPR, DC cardioversion, and if needed IABP.
Conflict of Interest:
None
MULTISTAGED MULTIVESSEL INTERVENTION DURING PRIMARY ANGIOPLASTY FOR EXTENSIVE ANTERIOR MYOCARDIAL INFARCTION
By Deepak Natarajan
Monday, November 22, 2010
Operator(s):
Deepak Natarajan
Affiliation:
Moolchand MedCity, New Delhi, India
Facility:
Department of Interventional Cardiology
Moolchand MedCity, New Delhi, India
History:
A 59 year old non diabetic, non hypertensive male was admitted for crushing chest pain radiating to both arms, accompanied by perspiration for the previous one hour. His EKG revealed extensive anterior myocardial infarction with bifascicular block (Figure 1).
Angiography:
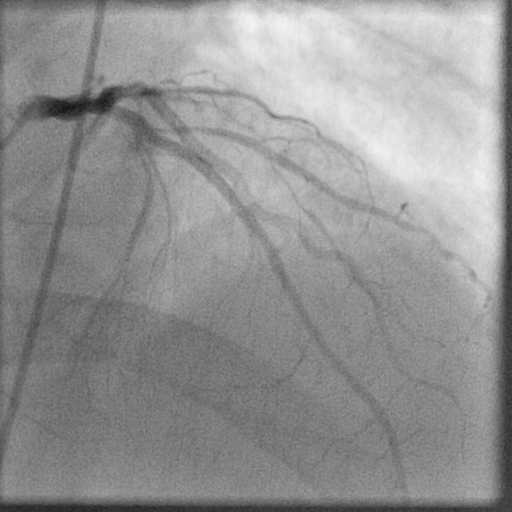
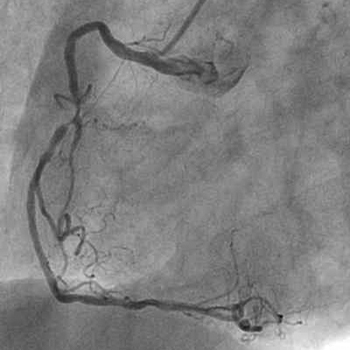
1) Left Main: normal
2) Left Anterior Descending Artery (LAD): 100% occlusion near ostium (Figure 2 and Figure 3)
3) Left Circumflex Artery (LCX): Mild disease
4) Right Coronary Artery (RCA): 85% mid vessel stenosis (Figure 4)
Procedure:
The left coronary artery ostium was engaged with a 6Fr left EBU guiding catheter and a 0.014″ BMW guidwire that was negotiated across the LAD occlusion. An intracoronary tirofiban bolus of 20mcg/Kg was administered, and repeated manual thrombus extraction was attempted using an Export catheter (Figure 5 and Figure 6). There was, however, little response in antegrade flow despite 6 attempts with the extraction catheter and repeat intracoronary tirofiban bolus of 10mcg/Kg. (Figure 7 and Figure 8). The patient was moved out of the cath lab into the coronary care unit, and intravenous tirofiban was infused at 0.15mcg/Kg/minute for the next 2 hours. The patient was wheeled back to the cath lab, and predilation was performed using 2.5x16mm and a 3x18mm balloons at 12atm (Figure 9and Figure 10). A long residual stenosis was apparent (Figure 11 and Figure 12), but reasonably brisk antegrade flow was achieved. Subsequently a 3.5x23mm everolimus-eluting stent (Xience) was deployed at 20atm (Figure 13). Angiography revealed TIMI 3 flow with minimal residual stenosis (Figure 14). The EKG revealed substantial improvement of the ST segments and disappearance of the bifascicular block (Figure 15).
It was decided to tackle the RCA lesion on a later occasion because the patient was hemodynamically stable and the procedure had been prolonged. Hence, after 6 weeks his left coronary artery system appeared disease free (Figure 16), but the RCA stenosis persisted (Figure 17). The RCA was engaged with a 6 ]Fr JR guiding catheter with side holes. A 0.014″ BMW gjidewire was negotiated through the stenosis; and following predilation with a 2x10mm balloon, a 3×12 sirolimus-eluting stent (Yukon) was deployed at 18atm (Figure 18). There was no residual stenosis and TIMI 3 flow was obtained (Figure 19 and Figure 20).
Conclusion:
The patient received continuos IV tirofiban infusion subsequently for 18 hours. The patient was discharged on both occasions on aspirin, clopidogrel, cilostazol, atorvastatin, ramipril, and metoprolol.
Comments:
Primary angioplasty is the treatment of choice in the majority of patients. There are, however, instances when the operator is confronted with other affected arteries besides the infarct-related vessel. The majority of interventional cardiologists are currently of the opinion that in the absence of hemodynamic instability, it is prudent to stage the procedure in multivessel disease. The interval can extend from while the patient is still hospitalized to as late as 8 weeks. This patient presented with an extensive anterior myocardial infarction (accompanied by a bifascicular block on his EKG) that necessitated a prolonged procedure involving large quantities of contrast. The index procedure was itself staged because there was little-to-no response to repeated manual thrombus extraction and IC tirofiban. The patient, therefore, was treated after 2 hours of IV tirofiban infusion. A recent New York Sate Registry has reported that patients undergoing staged multivessel intervention within 2 months after STEMI, but not during the index procedure had significantly less mortality.
Conflict of Interest:
None
PRIMARY PCI FOR ACUTE INFEROLATERAL MYOCARDIAL INFARCTION WITH SUSTAINED MONOMORPHIC VENTRICULAR TACHYCARDIA
By Deepak Natarajan
Monday, July 12, 2010
Operator(s):
Deepak Natarajan MD, Hakim Udin MD,Nirmalya Mukherjee MD and CK Krishna MD
Affiliation:
Moolchand MedCity, New Delhi, India
Facility:
Department of Interventional Cardiology
Moolchand MedCity
New Delhi, India
History:
A 76 year old non-diabetic, non-hypertensive man was admitted in the ER for central chest pain for the previous hour. His 12 lead ECG revealed a sustained monomorphormic ventricular tachycardia at a rate of 150 to 160 per minute of right bundle branch morphology (Figure 1, Figure 2). He maintained a systemic blood pressure of 90 mmHg. On reversion to sinus rhythm by 2 bolus injections of 150 mg amiodarone, an acute inferolateral myocardial infarction (ST segment elevation in L 2, L3, AVF, and V5-V6) with marked ST segment depression in V1 to V3 was observed (Figure 3).
Angiography:
1) LM normal
2) LAD 50% mid vessel stenosis (Figure 4)
3) LCX 100% occluded
4) RCA multiple 50% stenoses and a long segment 90% PDA stenosis (Figure 5)
Procedure:
The left coronary artery was engaged by a 6Fr 3.5 XBU guiding catheter, and a CrossIt 100 guidewire was negotiated across the total occlusion (Figure 6). After manual thrombo suction by a 6Fr Export catheter and intracoronary tirofiban ( 25 mcg/Kg) bolus injection, a tight residual stenosis was seen. A 2.75x12mm sirolimus eluting stent was deployed at 18atm. Brisk antegrade TIMI 3 flow was achieved with no residual stenosis (Figure 7).
Conclusion:
There was rapid disappearance of chest pain and near complete resolution of ST segment elevation in the inferolateral leads suggesting good myocardial perfusion (Figure 8). 2D echocardiogram demonstrated inferior wall hypokinesia with global ejection fraction of 50%. The patient was maintained on adequate oxygenation, and his serum potassium and magnesium levels were within normal limits. The patient was discharged 3 days post-admission on oral amiodarone . He did not receive any IV infusion of amiodarone.
Comments:
Primary sustained ventricular tachycardia is usually polymorphic and carries worse in hospital prognosis than patients without ventricular tachycardia. However, there is no increased recurrence or sudden death at one year follow up. The patient did not receive an ICD as patients surviving sustained primary VT have similar survival as patients who do not have primary VT. Moreover, this patient had an LV ejection fraction of 50% immediately post-PCI. Prompt revascularization by salvaging substantial myocardium and preventing recurrent ischemia aids in rectifying the electrical instability that accompanies acute MI.
Conflict of Interest:
None
POSSIBLE SYNERGISTIC EFFECTS OF INTRACORONARY TIROFIBAN AND MANUAL THROMBECTOMY IN ST ELEVATION ANTERIOR MYOCARDIAL INFARCTION
By Deepak Natarajan
Monday, April 05, 2010
Operator(s):
Deepak Natarajan, Mriganka Bharali, CK Krishna and Nirmalya Mukherjee
Affiliation:
Moolchand MedCity
New Delhi, India.
Facility:
Department of Interventional Cardiology
Moolchand MedCity
New Delhi, India
History:
A 50 year old non-diabetic, non hypertensive, and non smoking man was admitted in the emergency with severe chest pain of one hour duration. His 12 lead ECG revealed acute anterior ST elevation myocardial infarction (STEMI) (Figure 1). He had basal crackles and soon began having frequent short runs of ventricular tachycardia that necessitated 2 bulus injections of lignocaine.
Angiography(via the radial artery):
1) Normal left main
2) Left anterior descending (LAD) Artery totally occluded proximally (Figure 2)
3) Normal left circumflex artery (LCX) (Figure 3)
4) Normal right coronary artery (RCA) (Figure 4)
Procedure:
The left coronary artery was engaged by a 6Fr EBU guiding catheter, and a BMW 0.014 inch was initially used to cross the occlusion. The BMW guidewire kept slipping into the diagonal branch adjacent to the LAD occlusion. A CROSS-IT 100 guidewire was subsequently negotiated across the total LAD occlusion, and a bolus of intracoronary (IC) tirofiban was administered in 1 minute (25 mcg/Kg). This was followed by predilation by a 2x12mm balloon (Figure 5). A 6 Fr Export catheter for manual thombus suction was next deployed twice because of significant thrombus burden and sluggish flow following IC rirofiban and predilation (Figure 6, Figure 7). Manual thrombosuction resulted in TIMI 3 flow with minimal residual visible thrombus (Figure 8). The procedure was completed by the deployment of a 3x18mm Yukon DES at 18atm (Figure 9). Brisk TIMI 3 antegrade flow was achieved with no residual stenosis (Figure 10,Figure 11)
Conclusion:
There was rapid disappearance of chest pain with restoration of epicardial LAD blood flow and near complete resolution of ST segment changes in less than 60 minutes suggesting excellent myocardial reperfusion (Figure 12). Intravenous tirofiban was continued for 24 hours; and the patient discharged on 150mg aspirin, 150mg clopidogrel, and 200mg of cilostazol.
Comments:
There is limited to no data on IC glycoprotein 2b/3a blockers administered in STEMI. A small German randomized study concluded that IC abciximab in STEMI resulted in smaller infarcts, less microvascular obstruction, and better perfusion compared to intravenous abciximab. Another smaller study employing IC eptifibatide in patients with acute coronary syndrome revealed more local receptor occupancy by IC eptifibatide and better microvascular reperfusion. This study did not include patients with STEMI requiring primary PCI. Manual thrombus extraction has been shown by the TAPAS and EXPIRA studies to reduce infarct size and mortality. The technique is safe, effective, and easy to perform.
This case report highlights the need for more randomized studies to establish the synergistic effect of combining IC tirofiban with thrombosuction in patients with STEMI.
The single most effective technique to significantly reduce bleeding at access site is the radial approach which was used in this patient.
Conflict of Interest:
None
Intracoronary Tirofiban With Plain Balloon Angioplasty For Subacute Stent Thrombosis
Balloon Angioplasty for RCA In-stent Restenosis and Cross-Over Stenting for Unprotected Distal LMCA - Ostial LAD Stenoses
By Deepak Natarajan
Monday, May 11, 2009
Operator(s):
Deepak Natarajan MD, DM
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Department of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
History:
A 75 year-old hypertensive male with left lung upper lobe resection for carcinoma in 1997 and PCI with stenting of his right coronary artery (RCA) with a bare metal stent (BMS) in 2002 was admitted for unstable angina and shortness of breath for the past 5-6 days. His ECG revealed right bundle branch block with ischemic ST segment changes. The troponin-I was significantly raised. The 2-D echocardiogram demonstrated mild apical left ventricular (LV) hypokinesia with a global LV ejection fraction of 54%.
Angiography:
- LM: distal 60% eccentric stenosis


- LAD: ostial 90% stenosis with additional 70% proximal stenosis.
- LCX: no disease
- RCA: 80-90% BMS restenosis

Procedure:
The RCA was engaged first with a 6Fr JR guiding catheter, and a Hi-Torque Whisper MS guidewire was negotiated through the in-stent restenotic lesion and sequential balloon angioplasty attempted with 1.5x12mm,2x12mm,2.5x10mm, and finally 3.5x15mm balloons inflated to 14atm  achieving TIMI 3 flow with minimal residual stenosis
achieving TIMI 3 flow with minimal residual stenosis 
The left coronary artery was next engaged with a 7Fr EBU guiding catheter with a 3.5cms curve, and a Whisper guidewire placed into the distal LAD artery while an ATW 0.014 inch floppy guidewire was positioned in the LCX. The LAD stenoses were predilated sequentially with 2x12mm and 2.5x12mm balloons.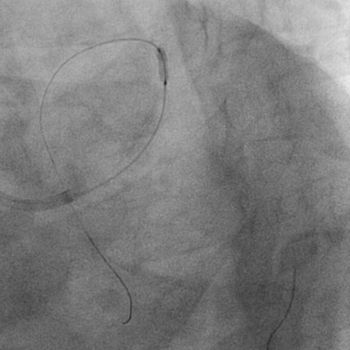 A 3.5x32mm TAXCOR paclitaxel-eluting stent (PES) was deployed from the LMCA to the proximal LAD across the LCX
A 3.5x32mm TAXCOR paclitaxel-eluting stent (PES) was deployed from the LMCA to the proximal LAD across the LCX 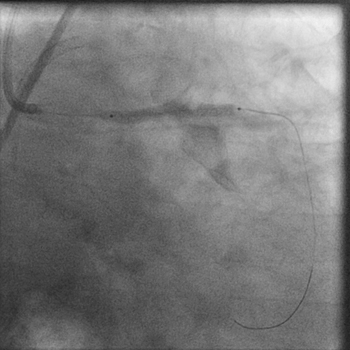 initially at 12 atm. Subsequently the LCX guidewire was removed, and the PES further inflated to 18atm. A 3.5x10mm noncompliant balloon was next used for post-dilation at 24atm.
initially at 12 atm. Subsequently the LCX guidewire was removed, and the PES further inflated to 18atm. A 3.5x10mm noncompliant balloon was next used for post-dilation at 24atm. 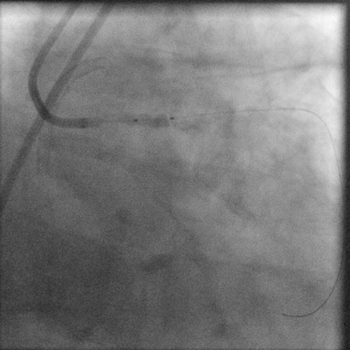 TIMI 3 flow was obtained in the left coronary arterial system with no residual stenosis or dissection. There was absolutely no jailing of the LCX and therefore no kissing balloon was performed.
TIMI 3 flow was obtained in the left coronary arterial system with no residual stenosis or dissection. There was absolutely no jailing of the LCX and therefore no kissing balloon was performed. 
Conclusion:
His further stay in the hospital was uneventful, and he was discharged after 2 days on triple anti-platelet therapy consisting of aspirin, clopidogrel, and cilostazol.
Comments:
Percutaneous coronary intervention in unprotected LMCA lesions with drug-eluting stents is emerging as an alternative to CABG. The large SYNTAX randomized study comparing PCI with CABG in LMCA and 3 vessel disease has suggested that results with PCI are comparable to CABG especially in the subsets of isolated LMCA ir LMCA with single vessel disease (N Engl J Med. 2009;360:961-72). Another large observational study from 4 French centers involving 291 patients with unprotected distal left main lesions has reported excellent angiographic results and good mid term clinical outcomes with provisional side branch T stenting (Circulation 2009;119:2349-2356).
In this particular patient it was imperative that the RCA in stent restenosis was tackled first followed by cross-over stenting for the distal left main/ostial and proximal LAD lesions.
Conflict of Interest:
None
DIRECT STENTING OF AN ABERRRANT RCA ARISING FROM LEFT CORONARY SINUS CONFIRMED BY 64-SLICE MDCT
By Deepak Natarajan
Monday, February 09, 2009
Operator(s):
Deepak Natarajan, MD, DM and Sandeep Vohra, MD
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology and Radiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 65 year old hypertensive patient was admitted for Troponin T negative unstable angina. He was having retrosternal chest pain for the previous 5 days with radiation to left arm at rest and during exercise accompanied by perspiration. His ECG showed ST segment depression in the chest leads.
Angiography:
- LM was normal.
- LAD was normal
 The second diagonal branch (D2) was large with an 80% ostial stenosis extending to proximal segment of the vessel.
The second diagonal branch (D2) was large with an 80% ostial stenosis extending to proximal segment of the vessel. - LCX was normal
- RCA was aberrant and arising from the opposite left sinus of Valsalva (ARCAOS) with an 80% mid-segment stenosis.
 The ARCAOS was hooked using a 6Fr multipurpose diagnostic catheter.
The ARCAOS was hooked using a 6Fr multipurpose diagnostic catheter.
Procedure:
Two bolus injections of eptifibatide were administered I/V before the PCI procedures. The ARCAOS was intubated with a 6Fr JL guiding catheter, and a 0.014″ BMW guidewire was placed across the stenosis followed by direct stenting with a 2.5x15mm Taxcore paclitaxel-eluting stent at 16atm 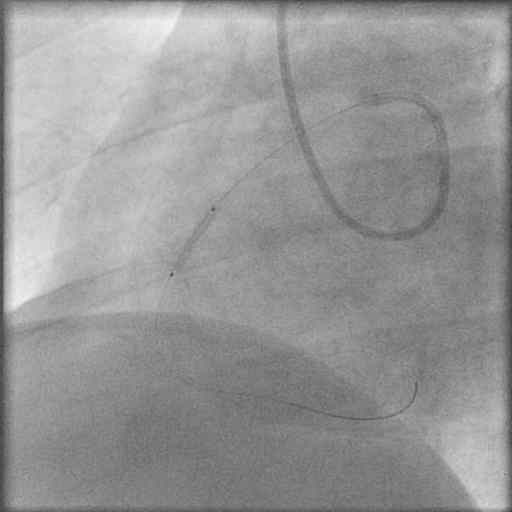 Brisk antegrade flow was achieved with no dissection or residual stenosis.
Brisk antegrade flow was achieved with no dissection or residual stenosis. 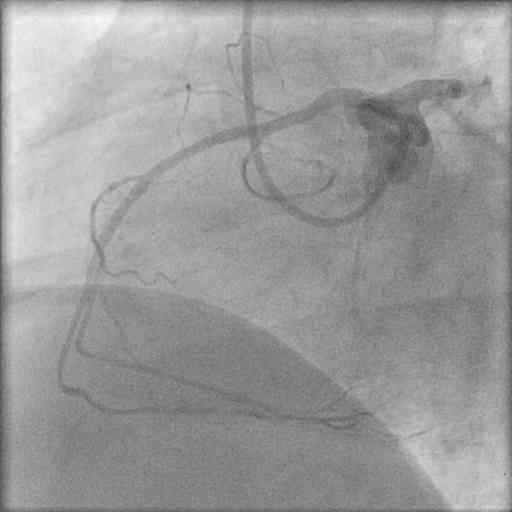
The left coronary artery was engaged with a 7Fr JL guiding catheter, and two floppy guidewires were positioned in LAD and D2. The D2 lesion was predilated with a 2x10mm Elect balloon, and a 2.5x12mm PRO-kinetic cobalt chromium was deployed at 14atm. 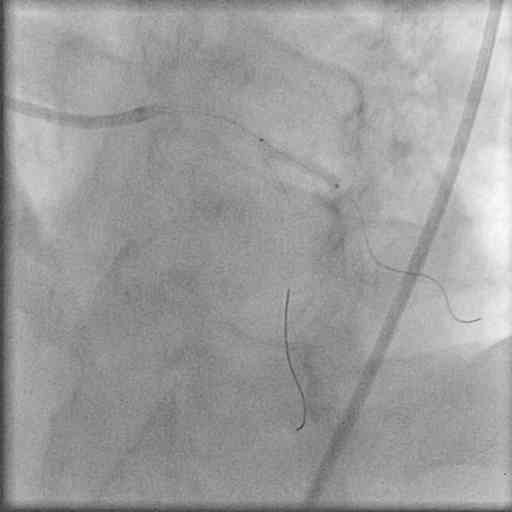 The procedure was completed with kissing balloon inflations
The procedure was completed with kissing balloon inflations  that ensured TIMI 3 flow without any residual stenosis or dissection.
that ensured TIMI 3 flow without any residual stenosis or dissection. 
Conclusion:
A 64- slice computerized tomography coronary angiogram (CTCA) confirmed the dominant right coronary artery arising from the left sinus of Valsava with a patent stent in the mid segment. Moreover, the ARCAOS was coursing between the aorta and pulmonary artery. 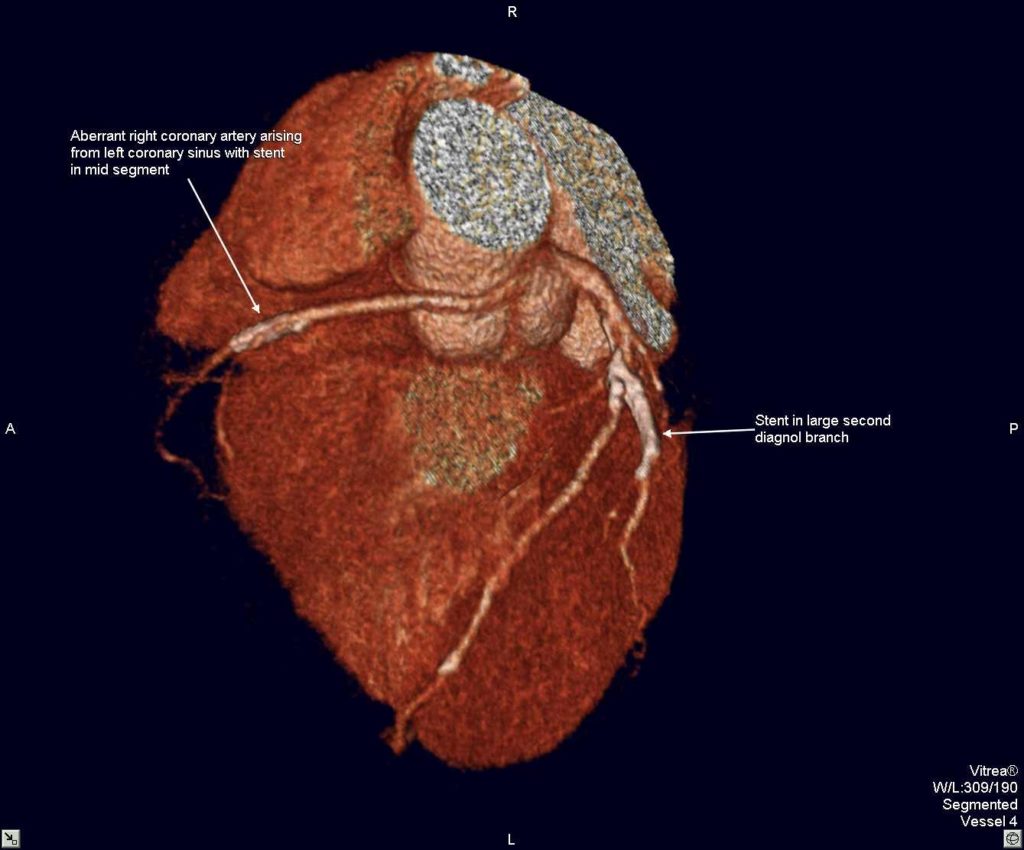
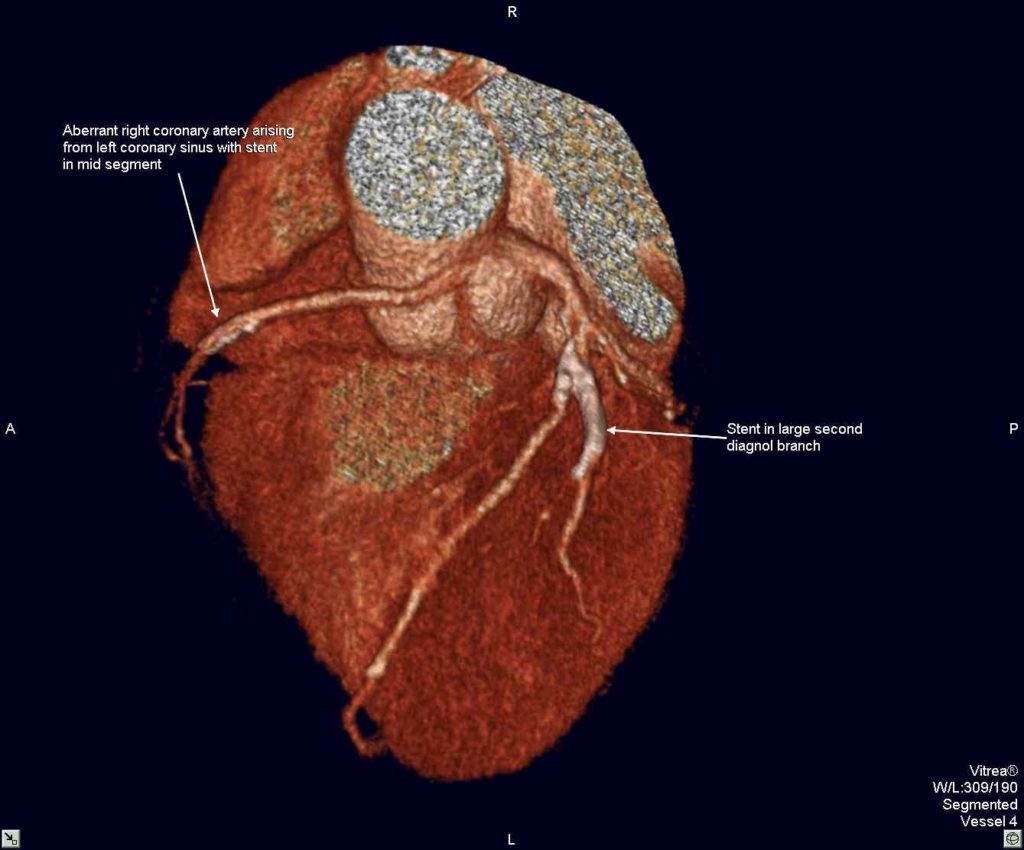
 The stent in D2 was also patent.
The stent in D2 was also patent.
Comments:
The exact pathophysiology resulting in life threatening cardiac ischemia continues to evolve albeit it is established that ARCAOS may result in sudden cardiac death. The incidence of coronary anomalies may be 5% and that of ARCAOS alone may as high as 1%. There is currently no formal protocol for screening aberrant coronary arteries in athletes and soldiers. Besides the scissoring effect of the great vessels on an ARCAOS producing significant ischemia, it has also been demonstrated that the initial portion of an ARCAOS can be compromised as it travels within the intramural aortic wall. This can best be determined by IVUS, and there is a report of PCI with stenting of the most proximal intramural part of an ARCAOS causing cardiac ishemic symptoms. This case demonstrates that in a symptomatic middle aged male with ARCAOS the cause of ischemia can be atherosclerosis and which may be easily managed by PCI.
Conflict of Interest:
NIL
PCI VIA RIGHT RADIAL ROUTE FOR IMPENDING ANTERIOR MI
By Deepak Natarajan
Monday, February 02, 2009
Operator(s):
Deepak Natarajan, MD, DM and Sandeep Vohra, MD
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 47 yr old uncontrolled type 2 diabetic with hypertension and a previous stent in his RCA was admitted for severe intermittent central chest pain for the past 12 hours. He was also having marked shortness of breath. His Troponin T was raised, and the ECG showed ST segment elevations in the anterior leads.
Angiography:
Done by the right radial artery approach using a 6 Fr Terumo sheath and a 6Fr Terumo TIG diagnostic catheter:
LM :OK
LAD: Tight proximal 75% long stenosis with large thrombus burden in the most proximal part of the stenosis 

LCX; Dominant vessel with a proximal ulcerated 85% stenosis 
RCA: Small vessel with patent previous stent in mid segment 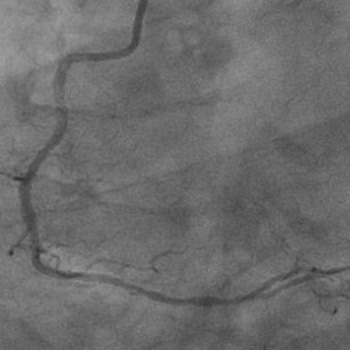 Procedure:
Procedure:
Following preloading with chewable 325mg of aspirin and 900mg of clopidogrel a 6Fr JL guiding catheter via the same radial sheath was used to engage the LCA and an All Star 0.014″ guidewire was put across the LAD stenosis that was sequentially predilated by a 2x10mm Elect balloon (Biotronik).  A 2.75x28mm Cypher Select stent
A 2.75x28mm Cypher Select stent  was deployed at 18atm to achieve TIMI 3 flow without dissection or residual stenosis.
was deployed at 18atm to achieve TIMI 3 flow without dissection or residual stenosis.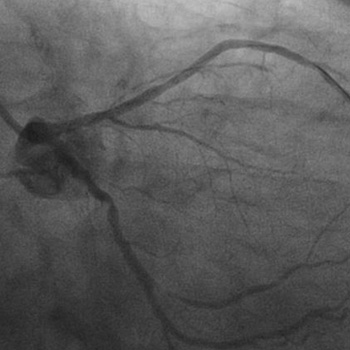 The same guidewire was repositioned in the LCX artery; and the stenosis predilated with a 2×10 mm Elect balloon followed by implantation of a 3x10mm Cypher Select stent 16atm
The same guidewire was repositioned in the LCX artery; and the stenosis predilated with a 2×10 mm Elect balloon followed by implantation of a 3x10mm Cypher Select stent 16atm 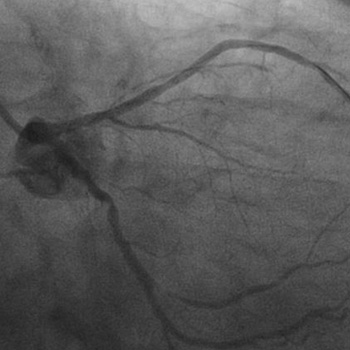 There was brisk antegrade flow with no residual stenosis or dissection.
There was brisk antegrade flow with no residual stenosis or dissection. 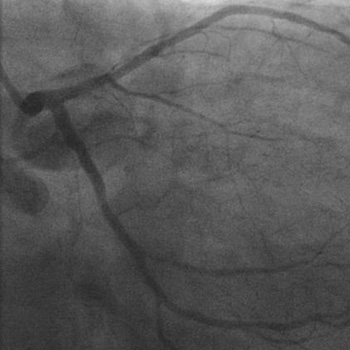
Conclusion:
TIMI 3 flow was achieved in both the LAD and LCX arteries without any residual stenosis nor any dissection. 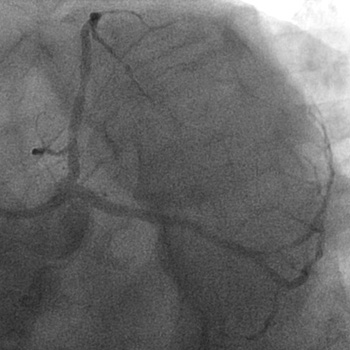
 The patient was maintained on injection eptifibatide. The patient’s pain and shortness of breath were relieved promptly subsequent to the PTCA/stenting of the LAD artery. He was discharged the next day on triple antiplatelet therapy consisting of 100mg of aspirin, 75mg of clopidogrel and 100mg of cilostazol twice a day.
The patient was maintained on injection eptifibatide. The patient’s pain and shortness of breath were relieved promptly subsequent to the PTCA/stenting of the LAD artery. He was discharged the next day on triple antiplatelet therapy consisting of 100mg of aspirin, 75mg of clopidogrel and 100mg of cilostazol twice a day.
Comments:
The severe intermittent chest pain accompanied by marked shortness of breath, elevated Troponin T levels, and significant ST segment elevation in the anterior precordial leads suggested an impending acute anterior MI. The tight proximal LAD stenosis with considerable visible thrombus burden indicated an on going myocardial infarction accompanied by a spontaneous thrombolysis/thrombogenesis. The presence of a large thrombus burden in the culprit vessel necessitated the administration of intracoronary bolus of eptifibatide. This case underscores the fact that the radial artery can be safely and effectively used in urgent complex interventions with minimal or no complications.
Conflict of Interest:
NIL
PRIMARY PCI FOR ACUTE ANTERIOR MYOCARDIAL INFARCTION IN PRESENCE OF CRITICAL LEFT MAIN CORONARY ARTERY STENOSIS
By Deepak Natarajan
Monday, September 08, 2008
Operator(s):
Deepak Natarajan (DM),Sarita Rao(DM),Vivek Prakash (DM)and Jasbir Singh (MD).
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Department of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
History:
A 77 year old hypertensive male who had sustained an old inferior myocardial infarction 24 years ago was admitted directly into the coronary intensive care unit with 5 days of severe recurring chest pain not responding to sublingual nitroglycerin. Soon after admission he developed severe prolonged chest pain not responding to i/v morphine and that was accompanied by marked EKG changes of new onset left bundle branch block and ST segment depression of 2 to 4 mms in leads 1, aVL,V2 to V6. There was also discordant ST elevation of 3mm in lead 3. 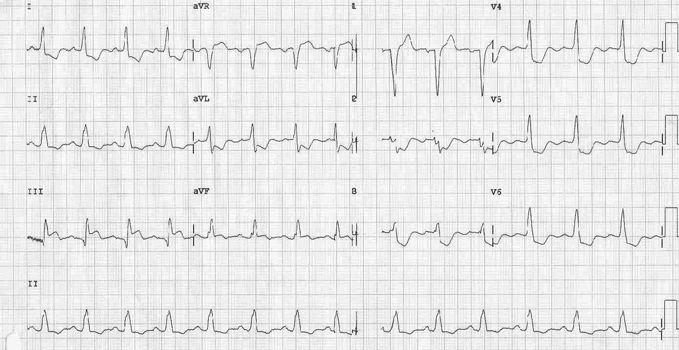 He rapidly became breathless with widespread crepitations in both lungs and began to lose systemic pressure. He was therefore quickly wheeled to the cath lab on dopamine support.
He rapidly became breathless with widespread crepitations in both lungs and began to lose systemic pressure. He was therefore quickly wheeled to the cath lab on dopamine support.
Angiography:
- Left Main 80% mid shaft stenosis.

- LAD artery 99% proximal stenosis with TIMI 2 flow.

- LCX 90% stenosis after a large intact OM 1.
- The left coronary system was providing a large collaterals to the RCA
 that was totally occluded.
that was totally occluded. 
Procedure:
In view of the ongoing acute anterior myocardial infarction (MI) and highly unstable hemodynamics (he was by then in frank pulmonary edema with systemic systolic pressure on dopamine of 80 to 90mmHg), the left coronary artery was engaged with a 6 Fr EBU left guiding catheter; and a 0.014″ floppy guidewire was negotiated across the LM and LAD stenoses. The LAD was predilated with a 2.0x12mm balloon at 14atm. 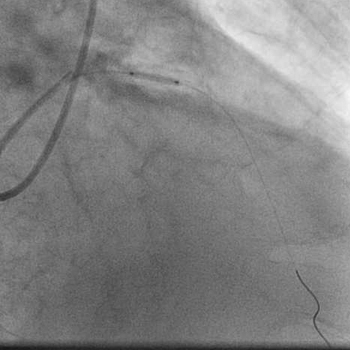 A 3.5x18mm cobalt chromium bare metal was next quickly deployed at 20atm in the LAD lesion.
A 3.5x18mm cobalt chromium bare metal was next quickly deployed at 20atm in the LAD lesion. 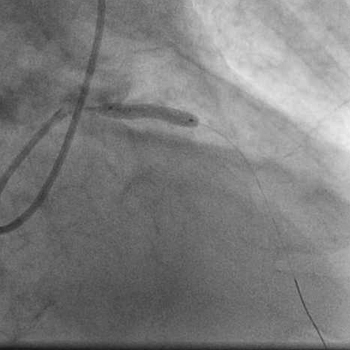 Angiogrpahy revealed TIMI 3 flow in the LAD artery with no residual stenosis or dissection.
Angiogrpahy revealed TIMI 3 flow in the LAD artery with no residual stenosis or dissection. 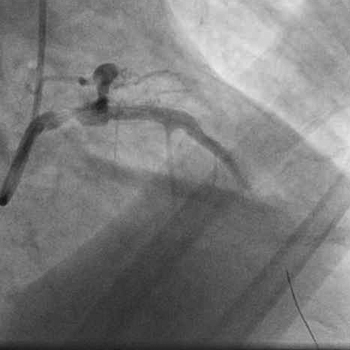 The same balloon was withdrawn into the left main and inflated at 18atm.
The same balloon was withdrawn into the left main and inflated at 18atm. 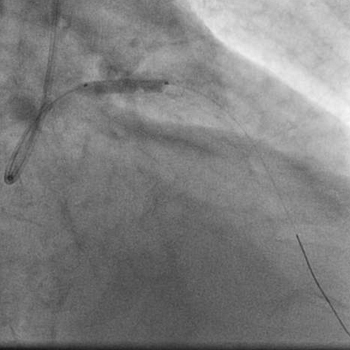 Angiography showed minimal residual stenosis of the left main artery with good TIMI 3 antegrade flow and no dissection.
Angiography showed minimal residual stenosis of the left main artery with good TIMI 3 antegrade flow and no dissection. 
Conclusion:
The patient’s chest pain was swiftly relieved following LAD stenting and balloon angioplasty of the left main coronary artery, and his pulmonary edema substantially resolved by next morning with parenteral furosemide. The dopamine drip was withdrawn completely by 72 hours. The ECG now displayed complete resolution of ST segments, normal QRS duration, and R waves from V2 to V6.  The patient subsequently underwent successful CABG with a LIMA and venous grafts. He was discharged on the tenth post-operative day.
The patient subsequently underwent successful CABG with a LIMA and venous grafts. He was discharged on the tenth post-operative day.
Comments:
This was a classic case of an evolving acute anterior MI. In view of the marked hemodynamic instability, the culprit vessel (proximal LAD artery) was not only dialted and stented with a BMS despite the presence of three vessel disease and a critical mid left main lesion. In order to ensure complete relief of myocardial ischemia, the left main coronary artery was also dilated, but not stented. Conventional protocols suggest that in the event of discovering left main or severe 3 vessel disease during primary PCI for an anterior MI the infarct related artery need only be dilated without stenting in order to allow subsequent CABG surgery. However, it also well recognized that following elective and primary balloon angioplasty, abrupt closure of the infarct-related artery, during or within hours of the procedure, can occur in 3% of the patients. This patient underwent stenting of his infarct-related LAD lesion to prevent any immediate or future recoil of the vessel as that would have been catastrophic. The patient was too unstable to permit stenting of the left main artery and hence it was thought prudent to merely dilate this vessel for immediate hemodynamic gain and prepare him for coronary bypass surgery that was successfully done 4 days after the index PCI procedure. The timing of CABG after restoration of antegrade flow in the culprit artery with primary PCI in patients with left main or severe multivessel coronary artery disease disease remains undefined.
Conflict of Interest:
None
CROSS OVER STENTING FOR OSTIAL LEFT ANTERIOR DESCENDING ARTERY STENOSIS INVOLVING DISTAL LEFT MAIN CORONARY ARTERY
By Deepak Natarajan
Monday, July 28, 2008
Operator(s):
Deepak Natarajan, Vivek Prakash and Jasbir Singh
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Department of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
History:
A 59 year old man was admitted for severe resting chest pain over last 2 weeks. Past medical history was significant for hypertension and heavy smoker for more than two decades. His baseline ECG revealed non specific ST-T wave changes accompanied with increase in serum troponin I levels. There was no family history of heart disease.
Angiography:
- LM: 95% distal Left main
- LAD: 95% Ostial stenosis extending from the distal LM. 85% proximal LAD stenosis
- LCX: Large calibrre with mo significant stenosis.


- RCA: Luminal irregularities in mid segment.
- LV: Ejection fraction of around 55%.
Procedure:
Subsequent to informed consent to PCI the left coronary artery was engaged by a 7F JL 3.5 guiding catheter and a 0.014″ floppy wire was advanced into the LAD across the lesions. Both lesions (distal LM to ostial LAD and the proximal LAD) were sequentially pre-dilated with 1.5×15 and 2×15 mm balloons 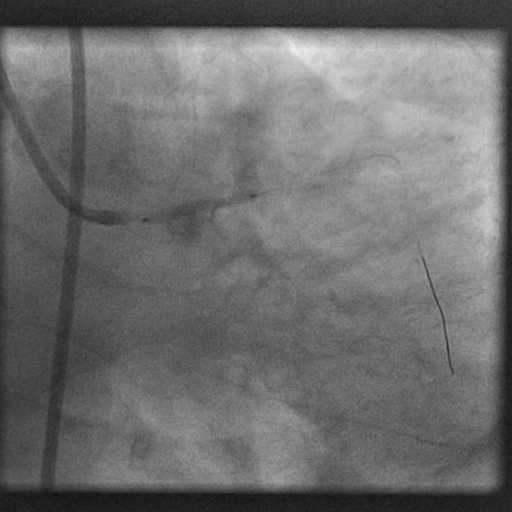 up to 14 atm. Following pre-dilatation a 3×32 mm paclitaxel eluting stent was placed from the most distal part possible of the LM artery into the LAD to cover the left main and both ostium and LAD proximal stenosis. This was deployed up to 20 atm.
up to 14 atm. Following pre-dilatation a 3×32 mm paclitaxel eluting stent was placed from the most distal part possible of the LM artery into the LAD to cover the left main and both ostium and LAD proximal stenosis. This was deployed up to 20 atm. 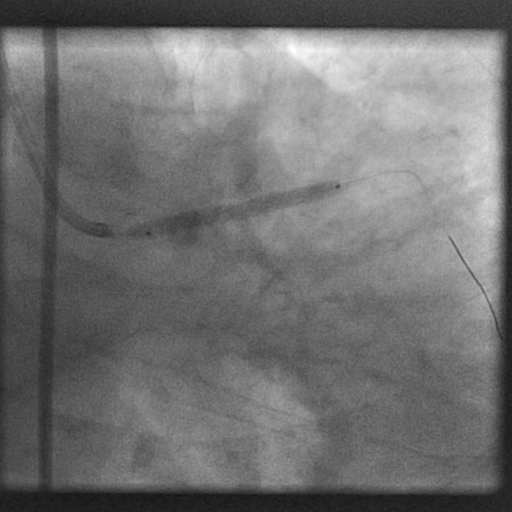 Additional postdialtation was performed with a 3.5×10 mm high pressure balloon up to 24 atm.
Additional postdialtation was performed with a 3.5×10 mm high pressure balloon up to 24 atm. 
 The final angiogram showed a fully expanded stent without residual stenosis or dissection. There was no compromise of the LCX artery.
The final angiogram showed a fully expanded stent without residual stenosis or dissection. There was no compromise of the LCX artery. 
Conclusion:
Cross over stenting is the simplest technique to employ in distal LM lesions not involving the left circumflex artery. In this case TIMI 3 flow was achieved with no complications.
Comments:
In this case the choice of cross over stenting was simple because there was no lesion in the circumflex artery. The approach for distal LM bifurcation not involving the left circumflex or a small / insignificant circumflex artery is cross over stenting from the LM to the LAD artery. In the event of jailing or compromise of the left circumflex post cross over stenting the situation should be dealt accordingly, usually with balloon angioplasty or another stent. The distal LM artery though involved was stenosed at its most distal tip adjacent to the LAD ostium. The procedure was quick and uncomplicated. The patient was discharged a day after procedure on triple antiplatelet therapy for the next one month and 2 days of injection fondaparinux.
Conflict of Interest:
None
INTERNAL CRUSH STENTING FOR RIGHT CORONARY ARTERY BIFURCATION STENOSIS
By Deepak Natarajan
Monday, June 30, 2008
Operator(s):
Deepak Natarajan(MD, DM) and Vivek Prakash(DM)
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
History:
A 69 yr old non diabetic male who had already received one bare metal stent each in his proximal LAD and mid RCA 4 years ago was readmitted for severe typical chest pain at rest, with ischemic ECG changes and positive troponin I values. On examination his heart rate was 60/min, blood pressure 180/110 mm Hg and he had a loud first sound with clearly audible S4. There was no evidence of heart failure.
Angiography:
His coronary angiogram revealed
Left main : normal.
LAD : Patent stent and rest of the vessel normal (Figure 1).
Left Cx ; Patent stent with non critical proximal lesion of 30%.
RCA ; Patent stent with 75 %to 90% stenosis involving the RCA/PDA bifurcation (Figure 2).
LV angiogram : Normal size LV with good LVEF of 60%.
Procedure:
The right coronary artery was engaged with a 7Fr JR guiding catheter and a floppy wire 0.014 was introduced across the lesion into the PDA. Following predilatation by a 2.0/15 mm balloon a 2.5/20 PES was deployed at 18 atm (Figure 3). Angiograms demonstrated no residual stenosis in the stent but a 90% ostial stenosis in the Postero-lateral branch secondary to the stent (Figure 4). A new hydrophilic wire was negotiated across the stent into the large PLV branch and the struts dilated with an 1.5/10 mm balloon. A 2.0/10 PES positioned with its proximal end 2mm within the MV for an internal crush (Figure 5). Following deployment of the SB stent at 16 atm and a repeat angio the SB stent was next crushed with a 2.5+20 balloon at 20 atm (Figure 6 and Figure 7). The side branch stent struts were expanded by a 2+10 mm balloon at 16 atm (Figure 8) and eventually kissing balloon angioplasty was employed to achieve excellent results (Figure 9).
Conclusion:
There was no residual stenoses or dissection (Figure 10 and Figure 11). The procedure was preceded by 2 bolus injections of eptifibatide. He was discharged after 2 uneventful days in the hospital on aspirin,clopidogrel,cilostazol and fondaparinux.
Comments:
Management of bifurcation lesions continue to evolve rapidly with the provisional stenting approach considered to be the best. As the PLV branch had no lesion this was a classic case for provisional stenting of the side branch. The internal crush should prove to be the easiest,safest and most logical approach in such lesions.
Conflict of Interest:
None
SIMULTANEOUS KISSING PACLITAXEL ELUTING STENTS FOR UNPROTECTED DISTAL LM LESION
By Deepak Natarajan
Monday, December 03, 2007, www.tctmd.com
Operator(s):
Deepak Natarajan MD, DM
Amit Malik MD, DM
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 72 year old obese female with long standing hypertension was urgently referred to the cardiac catheterization laboratory for repeated episodes of severe central chest pain accompanied by shortness of breath and perspiration at rest for the past 10 days. She had a family history of coronary artery disease, but did not have diabetes mellitus. Her electrocardiogram revealed marked ST segment depression in almost all leads.
Angiography:
- 80% distal left main (LM), 80% ostial left anterior descending (LAD) artery, and 90% ostial left circumflex (LCX) artery stenoses.

 The LM was a large 4.5 mm vessel.
The LM was a large 4.5 mm vessel. - The right coronary artery was also critically blocked.
- The left ventricular angiogram showed a normal sized ventricle with good contractions and ejection fraction of 56%.
Procedure:
The patient and her attendants consented to percutaneous intervention rather than CABG after being informed in detail of the pros and cons of both procedures. An intra aortic balloon pump was kept on stand by in the lab, and a temporary pacing lead was positioned in the right ventricular apex. The left coronary artery was engaged with a 7Fr JL 3.5 guiding catheter, and two 0.0014″ floppy guidewires were placed across the lesions in the LAD and LCX arteries. Both lesions were predilated by a 2.25x15mm balloon sequentially 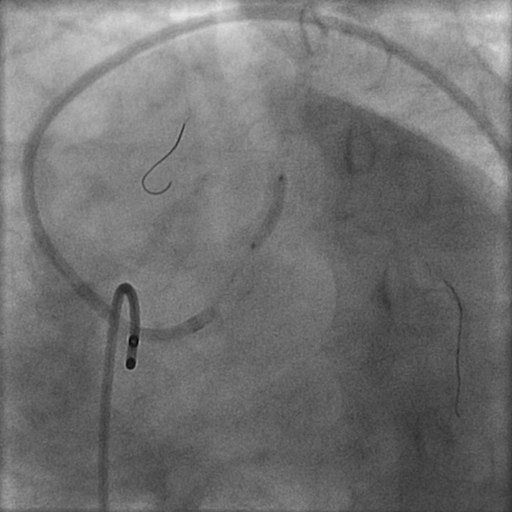
 with the balloon placed across the LM. Next two 3mm Paclitaxel-eluting stents were advanced one by one into the LAD (3×23 mm) and the LCX (3×15 mm) arteries; and both stents were pulled back into the LM artery in order to completely cover the LM lesion.
with the balloon placed across the LM. Next two 3mm Paclitaxel-eluting stents were advanced one by one into the LAD (3×23 mm) and the LCX (3×15 mm) arteries; and both stents were pulled back into the LM artery in order to completely cover the LM lesion.  After confirming the position of both stents, they were deployed with simultaneous inflations at 16atm.
After confirming the position of both stents, they were deployed with simultaneous inflations at 16atm. 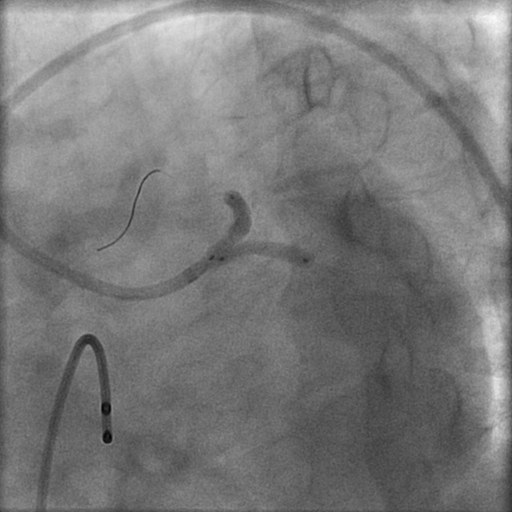 This was followed by sequential dilations of the LAD and LCX stents at 18atm.
This was followed by sequential dilations of the LAD and LCX stents at 18atm. 
 Next kissing balloon was done by simultaneous dilation of 2 balloons at 12atm.
Next kissing balloon was done by simultaneous dilation of 2 balloons at 12atm. 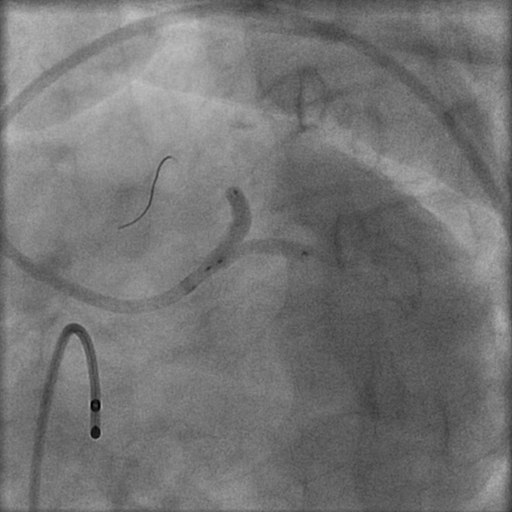 . The patient had been preloaded with aspirin plus clopidogrel and received standard bolus dose of Eptifibatide before the procedure along with unfractionated heparin, and the intervention was followed by 24 hour Eptifibatide infusion.
. The patient had been preloaded with aspirin plus clopidogrel and received standard bolus dose of Eptifibatide before the procedure along with unfractionated heparin, and the intervention was followed by 24 hour Eptifibatide infusion.
Conclusion:
There was TIMI 3 flow and no residual stenosis or dissection in any vessel. 
 There were no complications. The entire procedure was over within 20 minutes.
There were no complications. The entire procedure was over within 20 minutes.
Comments:
Drug eluting stents (DES), in conjunction with advances in peri and post procedural pharmacotherapies, have demonstrated the feasibility and efficacy of percutaneous intervention in unprotected left main coronary artery stenosis. In the recently concluded TCT 2007, the LE MANS randomized study comparing PTCA and stenting with CABG in unprotected left main stenosis demonstrated that stenting is not only safe and feasible for treatment of left main artery disease, but may also achieve better functional outcome than CABG. The 52 patients randomized to stenting had significant increase in left ventricle ejection fraction, and there was no difference in mortality or target vessel revascularization between the two treatment cohorts. More than a half (58%) of the patients had distal left main disease in the stenting group. A multicenter registry has recently recorded that percutaneous coronary intervention with DES in non bifurcation left main coronary artery disease appears safe with a restenosis rate of 0.9 %, long term major adverse clinical event rate of 7.4%, and a cumulative cardiac mortality of 2.7% at a median follow-up of 886 days. Bifurcation left main stenting, however, remains a challenge; but better stent platforms, novel procedural techniques, and optimal pharmacotherapies will further improve outcomes. Large randomized trials comparing DES to CABG such as the Synergy Between Percutaneous Intervention with TAXUS and Cardiac Surgery (SYNTAX) will provide answers to the uncertainties that remain with LM stenting. In this particular case the large left main artery necessitated the Simultaneous Kissing Stent technique as opposed to the Pull Back T Stenting method.
Conflict of Interest:
None
MULTIVESSEL STENTING INCLUDING BIFURCATION STENOSIS
By Deepak Natarajan
Monday, July 23, 2007, www.tctmd.com
Operator(s):
Deepak Natarajan MD, DM
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 58 year old male presented with non ST elevation myocardial infarction. He was a heavy smoker, but was not hypertensive or diabetic. The 12 lead EKG revealed ST-segment depression in the precordial leads and Troponin-T was positive. The previous day he had experienced near collapse accompanied by sternal chest pain and perspiration.
Angiography:
- 75%-80% proximal LAD stenosis.

- 70% proximal LCX stenosis.

- 90% stenosis of the mid RCA adjacent to the origin of a large right ventricle branch.
Procedure:
The left coronary artery was engaged with a 6Fr JL guiding catheter, and a 0.0014″ floppy guidewire negotiated across the LAD stenosis that was predilated with a 2.0x15mm balloon;  and an everolimus-eluting stent (Xience) 3.0x18mm was deployed at 18atm.
and an everolimus-eluting stent (Xience) 3.0x18mm was deployed at 18atm. 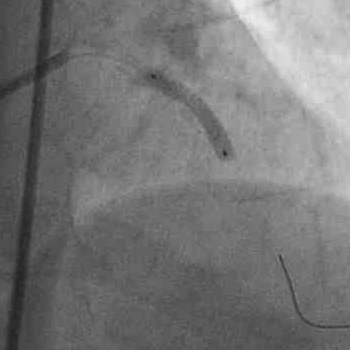 There was no residual stenosis and TIMI 3 flow was achieved.
There was no residual stenosis and TIMI 3 flow was achieved.  The same guidewire was then positioned in the LCX and the lesion stented with a bare metal ( Vision) stent 3.0x15mm at 18atm.
The same guidewire was then positioned in the LCX and the lesion stented with a bare metal ( Vision) stent 3.0x15mm at 18atm.  Angiography showed excellent flow into the LCX without any dissection.
Angiography showed excellent flow into the LCX without any dissection.  The RCA was next engaged with a 6Fr JR guiding catheter. Two floppy 0.0014″ guidewires were negotiated into the distal RCA and the right ventricle branch.
The RCA was next engaged with a 6Fr JR guiding catheter. Two floppy 0.0014″ guidewires were negotiated into the distal RCA and the right ventricle branch.  The RCA stenosis was predilated with a 2.0x15mm balloon; and a 2.5x18mm bare metal stent (BMS, Vision) was positioned across the lesion. Before inflating the stent, the guidewire in the right ventricle branch was removed;
The RCA stenosis was predilated with a 2.0x15mm balloon; and a 2.5x18mm bare metal stent (BMS, Vision) was positioned across the lesion. Before inflating the stent, the guidewire in the right ventricle branch was removed;  and the BMS deployed at 19atm.
and the BMS deployed at 19atm.  The final angiogram did not show any significant residual stenoses or dissection of either the main RCA or right ventricle branch.
The final angiogram did not show any significant residual stenoses or dissection of either the main RCA or right ventricle branch. 
Conclusion:
It was possible to achieve excellent flow in all 3 major vessels without any complications. The side branch of the RCA was not compromised. The patient was discharged the next day.
Comments:
The ARTS 11 and ERACI 111 studies comparing multivessel stenting involving DES with CABG have demonstrated comparable MACCE at follow up as for long as 3 years. The ARTS 11 trial used an average of 3.7 drug eluting stents with an average length of 73mm. The present case is an illustration of multivessel stenting utilizing one DES and 2 bare metal stents. the results were quite reasonable and there were no complications. Moreover, the tight bifurcation stenosis of the RCA could be managed with a single stent in the main vessel. The side branch was a little over 2mm; therefore, provisional stenting was never on the agenda, but in the event of significant residual stenosis or dissection of the side branch balloon angioplasty would have been possible. The SYNTAX and other ongoing randomized trials comparing multivessel stenting in 3 vessel disease with CABG should shed further light on multivessel stenting.
Conflict of Interest:
None
BARE METAL CORONARY STENTING OF ANAMOLOUS LEFT CIRCUMFLEX ARTERY
By Deepak Natarajan
Monday, February 26, 2007, www.tctmd.com
Operator(s):
Deepak Natarajan MD, DM
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 66 year old hypertensive lady had undergone stenting of her mid right coronary artery (RCA) in 2001. She was on eltroxin for hypothyroidism and was admitted in the ER this time for chest pain at rest and on exertion for the preceding 2 weeks.
Angiography:
- Normal left anterior descending artery (LAD).
- Normal right coronary artery (RCA).

- The left circumflex (LCX) artery was anomalous and was seen to be arising from the right coronary sinus very close to the origin of the RCA and had a tight 75% ostial stenosis.

Procedure:
The LCX was canalized with a 6Fr AR1 guiding catheter, and a 0.0014″ All Star guidewire was advanced across the LCX lesion.  Direct stenting was done using a Multilink Vision bare metal stent 3x12mm at 16atm.
Direct stenting was done using a Multilink Vision bare metal stent 3x12mm at 16atm. 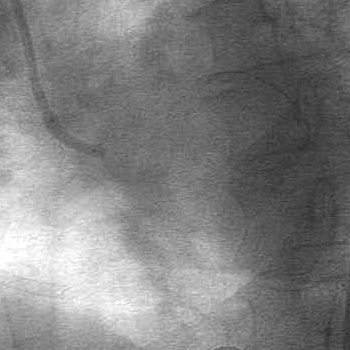 The patient had been maintained on nitroglycerin infusion throughout the procedure and received a bolus of eptifibatide immediately before stenting.
The patient had been maintained on nitroglycerin infusion throughout the procedure and received a bolus of eptifibatide immediately before stenting.
Conclusion:
TIMI 3 flow was achieved and there was no residual stenosis. 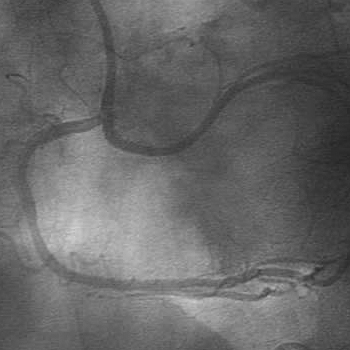
Comments:
Coronary artery anatomic variations are uncommon and have been seen in approximately 0.6-1.6% of patients undergoing coronary angiography. The aberrant LCX from the RCA or the right coronary sinus is the most common anomaly observed and usually discovered by chance during coronary angiography or at autopsy. It is considered benign as it causes no myocardial compromise. However, it becomes important for the cardiac surgeon in case of aortic valve replacement. In the event of substantial atherosclerosis, the presentation may be as an acute myocardial infarction or unstable angina, as in this case. Percutaneous coronary intervention may be simple and effective in both instances.
Conflict of Interest:
None
CORONARY DISSECTION FOLLOWING CRUSH STENTING FOR BIFURCATION STENOSIS
By Deepak Natarajan
Monday, August 21, 2006, www.tctmd.com
Operator(s):
Deepak Natarajan MD, DM
Affiliation:
Indraprastha Apollo Hospitals,New Delhi
Facility:
Departments of Cardiology
Indraprastha Apollo Hospitals, New Delhi, India
History:
A 59 year-old man was admitted to our service for unstable angina. He was a known hypertensive and had recently undergone an exercise ECG test which was strongly positive. He was not a diabetic and had stopped smoking a couple of years back. His LDL cholesterol was 150 mg%.
Angiography:
His coronary angiogram revealed a 95% bifurcation stenosis at the origin of the posterior descending artery (PDA) from a dominant circumflex coronary (LCX) artery. 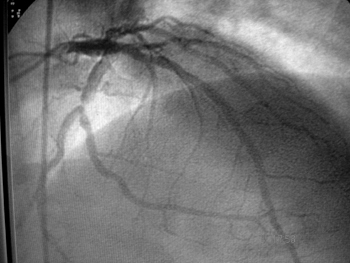 The left anterior descending artery (LAD) and the right coronary (RCA) arteries (non dominant) were normal.
The left anterior descending artery (LAD) and the right coronary (RCA) arteries (non dominant) were normal. 
Procedure:
The left coronary artery was engaged with a 7Fr Voda guiding catheter, and two 0.0014″ floppy guide wires were negotiated across the stenosis into the PDA and LCX arteries respectively. Following predilation with a 2x15mm balloon over both wires, a 3x18mm sirolimus eluting stent was positioned into the PDA while another 3x15mm sirolimus eluting stent was placed into the LCX artery. The PDA stent was placed slightly proximal to the LCX stent .  The LCX stent was first deployed at 14atm; and following a coronary angiographic injection, the wire was removed. Next the PDA stent was deployed at 14atm. The result was satisfactory with no complications.
The LCX stent was first deployed at 14atm; and following a coronary angiographic injection, the wire was removed. Next the PDA stent was deployed at 14atm. The result was satisfactory with no complications.  The floppy wire was renegotiated across the PDA stent struts and a 3x15mm balloon was inflated upto 16atm. Subsequent to this, kissing balloon inflations were performed.
The floppy wire was renegotiated across the PDA stent struts and a 3x15mm balloon was inflated upto 16atm. Subsequent to this, kissing balloon inflations were performed. 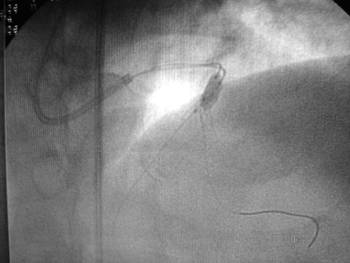 The balloons were inflated upto 12atm. Angiography revealed a significant dissection of the PDA distal to the stent.
The balloons were inflated upto 12atm. Angiography revealed a significant dissection of the PDA distal to the stent. 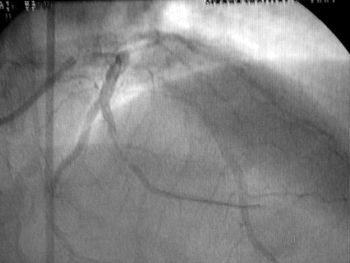 This was then predilated with a 2.5x15mm balloon and stented with a 2.75x15mm bare metal stent which was deployed at 16atm.
This was then predilated with a 2.5x15mm balloon and stented with a 2.75x15mm bare metal stent which was deployed at 16atm. 
Conclusion:
The final angiogram demonstrated TIMI 3 flow and no residual stenosis.  The patient was discharged the next day.
The patient was discharged the next day.
Comments:
Dissection of a coronary artery may develop following crush technique stenting. Although uncommon, it can be managed with deployment of an appropriate sized stent. In this case a bare metal stent was used for the sake of economy.
Conflict of Interest:
None