Dr. Deepak Natarajan
Director Interventional Cardiology
MBBS,MD,DM
DELHI, NCR


TORSEMIDE OR FUROSEMIDE FOR ACUTE HEART FAILURE ?
January 17, 2023
A recent study has brought greater clarity on which diuretic should be used in patients hospitalised with acute decompensated heart failure. Most clinicians would go with torsemide , considered stronger and more bioavailable than furosemide.
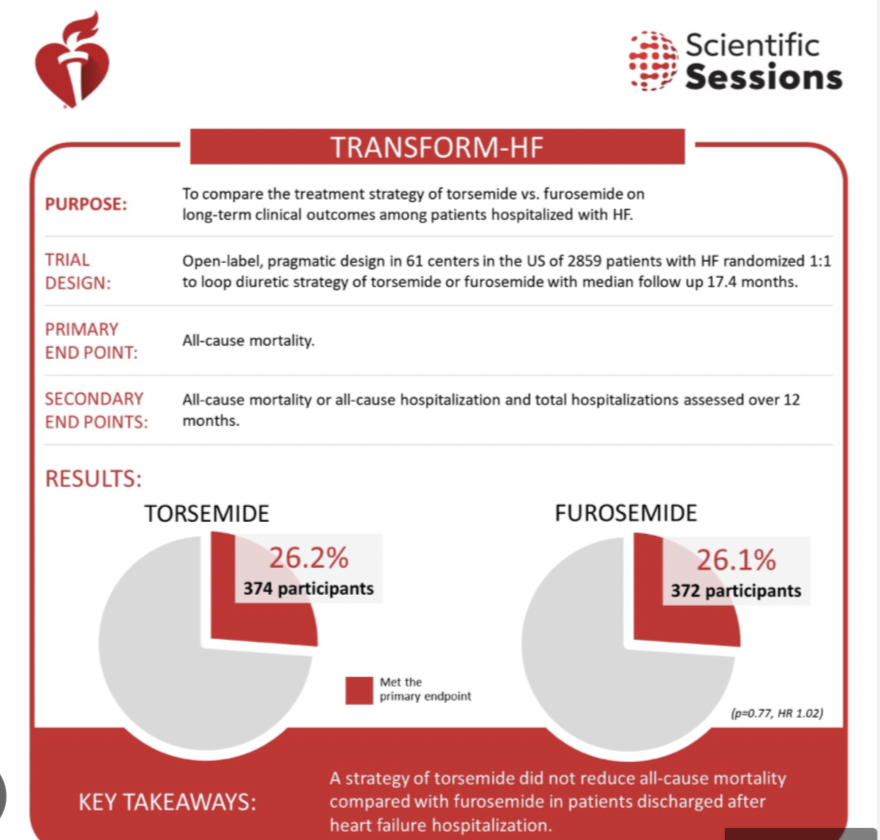
However the TRANSFORM-HF trial presented at the AHA 2022 in Chicago revealed that patients treated for heart failure (HF) with the loop diuretic torsemide had similar rates of death and hospitalization compared with those treated with furosemide, a more commonly prescribed diuretic. This is the first randomised trial comparing the 2 diuretics.
The trial enrolled patients hospitalized with worsening or new-onset HF with a plan for long-term loop diuretic therapy who had either an EF of 40% or lower or, regardless of EF, elevated natriuretic peptide levels when hospitalized.
Overall, 1428 were assigned to receive furosemide as their initial oral diuretic and 1431 patients were assigned to the torsemide-first strategy.
The pragmatic, open label study randomized 2,859 patients at more than 60 U.S. hospitals to either torsemide or furosemide. Of the participants, more than one-third were women, one-third were Black, and the median age was 65 years. Researchers also noted a broad range in the severity of HF ranging from recent diagnosis to worsening stages. Follow-up via phone was conducted at 30 days, six months and 12 months after hospital discharge.
The primary endpoint was all cause mortality, secondary endpoint was all cause mortality or all cause hospitalisation.
After a median of 17.4 months, results showed nearly identical mortality rates in both the torsemide (26.1%) and the furosemide (26.2%) groups. At 12 months, all-cause death and hospitalization rates were also similar in the torsemide (47.3%) and furosemide (49%.3) groups. Researchers noted the primary outcome demonstrating furosemide equivalence to torsemide was the same across all pre-specified subgroups including ejection fraction.
Either furosemide or torsemide are acceptable options for diuresis among hospitalised patients with heart failure, as there is little difference in clinical outcomes over year.
Treating physicians can continue starting such patients with HF on either agent, at their discretion, without concern that the choice may compromise outcomes.
Although furosemide is the most commonly used loop diuretic in HF, torsemide has both known and theoretical advantages that set it apart. Torsemide is more than twice as potent as furosemide and more bioavailable, and its treatment effect lasts longer.
Torsemide may have pleiotropic effects such as downregulating the renin-angiotensin-aldosterone system (RAAS), reduce myocardial fibrosis and promote reverse ventricular remodeling.
In practice, torsemide may be preferred in patients with furosemide resistance or challenges with bioavailability, especially in very advanced heart failure with gut edema, where oral furosemide is not effectively absorbed. Torsemide may be a better choice for individuals who have diuretic resistance with advanced congestion.
Despite theoretical advantage torsemide did not out perform furosemide in acute decompensated heart failure ; it is possible that certain patient groups may respond differently to these 2 diuretics. It is unlikely that there were Indians in the cohorts studied. Both drugs are manufactured in India , ands are quite cheap.
The researchers concluded that “Among patients discharged after hospitalization for heart failure, torsemide compared with furosemide did not result in a significant difference in all-cause mortality over 12 months. However, interpretation of these findings is limited by loss to follow-up and participant crossover and nonadherence.”
https://jamanetwork.com/journals/jama/article-abstract/2800428