Dr. Deepak Natarajan
Director Interventional Cardiology
MBBS,MD,DM
DELHI, NCR


ANTI PLATELET THERAPY AFTER CORONARY STENTING AND INTRACEREBRAL BLEED.
January 16, 2023
Recently a middle aged diabetic and hypertensive male who had been stented with an everolimus eluting tent in the left anterior descending coronary artery for unstable angina was admitted with acute onset of weakness in his left arm, and systolic blood pressure of 200 mm Hg. The patient was on DAPT consisting of clopidogrel and aspirin (75 mg each). A 128 slice CT scan of brain revealed a right thalamic bleed. The patient was admitted in intensive care, and DAPT stopped. A repeat CT scan did not show any progression in the bleed or cerebral oedema. There was modest improvement in power of his left arm.This time clopidogrel was resumed minus aspirin, with tight control of blood pressure. The patient was discharged on blood pressure therapy, injection Lantus insulin, and mono anti-platelet therapy ( clopidogrel 75 mg once a day).
The above case illustrates the dilemma faced by a treating cardiologist when a recently stented patient is admitted with a cerebral bleed. Continuing with DAPT risks aggravating the intra cerebral hemmorhage , while stopping anti platelets can result in acute stent thrombosis, which in turn could be lethal. There are no guidelines in management of such patients, apart from a few case reports.
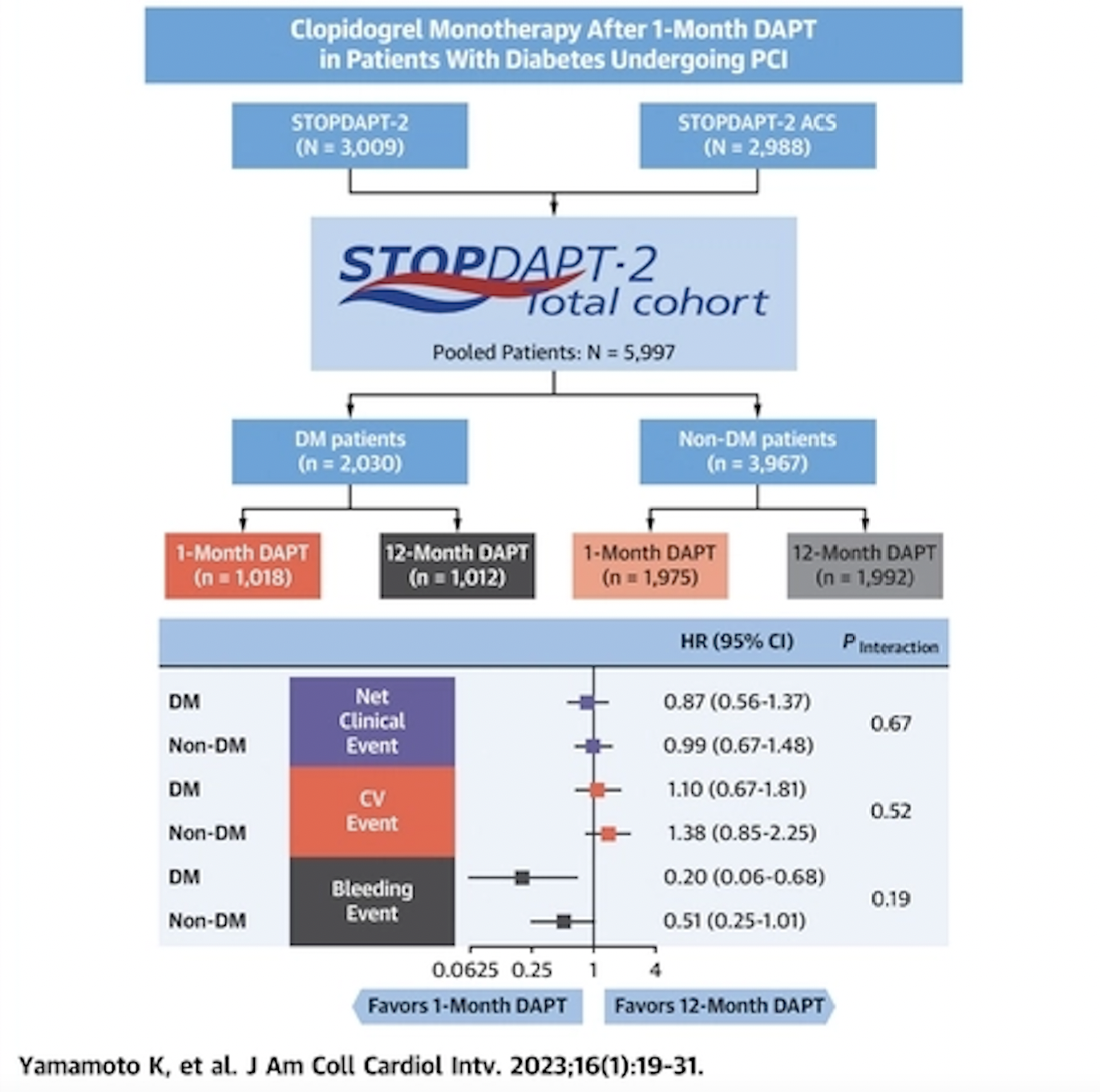
Some light is thrown by a Japanese paper published today in JACC:Cardiovascular Interventions (J Am Coll Cardiol Intv. 2023 Jan, 16 (1) 19–31). The study highlights that clopidogrel mono therapy after just one month of DAPT is safe and effective in patients with diabetes undergoing percutaneous coronary intervention (PCI).
There have been randomised trials showing it is possible to shorten DAPT subsequent to coronary stenting with no difference in cardiovascular outcomes , but significant reduction in bleeding complications.
The Japanese study is a subgroup analysis of the STOPDAPT-2 trial. The study focused on data from nearly 6,000 PCI patients, including 2,030 patients with diabetes and 3,947 patients without diabetes.
Patients with diabetes were older and more likely to have a higher BMI. They were also more likely to have a history of prior coronary revascularization, prior myocardial infarction, prior stroke, heart failure, anemia, chronic obstructive pulmonary disease, peripheral artery disease, chronic kidney disease, hypertension or hyperlipidemia.
All patients in the analysis were treated with an initial month of DAPT with aspirin and clopidogrel or prasugrel. Patients were then randomized to continue DAPT for up to 12 months or switch to clopidogrel monotherapy.
The study’s primary endpoint was a composite of cardiovascular events (cardiovascular death, myocardial infarction, definite stent thrombosis or stroke) and bleeding events after one year.
Overall, among patients with diabetes, that endpoint was seen in 3.58% of patients in the clopidogrel monotherapy group and 4.12% of patients in the 12-month DAPT group (p = 0.55) Among patients without diabetes, that endpoint was seen in 2.46% of patients in the clopidogrel monotherapy group and 2.49% of patients in the 12-month DAPT group (p=0.97)
Importantly, the authors noted that there was much less bleeding if the patient was treated with clopidogrel monotherapy (0.30%) as opposed to 12 months of DAPT (1.5%), ( p=0.01).
The limitations were that many eligible patients were not enrolled into the STOPDAPT-2 trial due to “physician choice or patient refusal,” and many of those patients may have faced a higher risk of experiencing a cardiovascular or bleeding event after PCI.
Hence patients in this study represent a somewhat lower risk population than those encountered in real clinical practice. The incidence of the cardiovascular and bleeding events in this study was very low.”
Additional studies are still necessary to determine the optimal monotherapy strategy for diabetic patients undergoing PCI.
The authors conclude “clopidogrel monotherapy after 1-month DAPT compared with 12-month DAPT reduced major bleeding events without an increase in cardiovascular events regardless of diabetes, although the cndings should be considered as hypothesis generating, especially in patients with acute coronary syndrome, because of the inconclusive result in the STOPDAPT-2 ACS trial. (Short and Optimal Duration of Dual Antiplatelet Therapy After Everolimus-Eluting Cobalt-Chromium Stent–2 ).
There is however little data on management of intra-cerebral bleed soon after coronary stenting. Such a patient should be considered a high risk bleed. One option would be to resume mono therapy with clopidogrel as soon as possible provided there is no increase in the bleed. Duration for discontinuation of anti platelet would depend on the individual case, it will have to be shorter in the event of a recent bleed, as chances of stent thrombosis are highest in the 4 to 6 weeks following the index procedure.
Crucially STOPDAPT-2 employed everolimus eluting stents, but GLOBAL LEADERS trial with biolimus eluting stents showed that among patients who underwent PCI with a biolimus-eluting stent, 1 month of DAPT followed by ticagrelor monotherapy for 23 months was noninferior, but not superior to 12 months of DAPT followed by aspirin monotherapy for 12 months. The composite outcome, components of the primary outcome, and major bleeding were similar between treatment groups (Franzone A, McFadden E, Leonardi S, et al. Ticagrelor Alone Versus Dual Antiplatelet Therapy From 1 Month After Drug-Eluting Coronary Stenting. J Am Coll Cardiol 2019;74:2223-34). No difference in bleeding complications could be explained by the greater potency of ticagrelor compared to clopidogrel.
The 3 year followup of the SMART CHOICE trial showed 3-month DAPT, followed by P2Y12 inhibitor monotherapy was associated with a lower risk of clinically relevant major bleeding than prolonged DAPT. Although the 3-year risk of ischemic cardiovascular events was comparable between the 2 groups, this result should be interpreted with caution owing to the limited number of events and sample size.Bleeding Academic Research Consortium (BARC) types 2–5 bleeding occurred in 3.2% of the shortened DAPT group and in 8.2% of the prolonged DAPT group. Major bleeding, BARC types 3–5, occurred in 1.2% of the shortened DAPT group and in 2.4% of the prolonged DAPT group.